Learning objectives
- Definition and signs and symptoms of rhabdomyolysis
- Causes of rhabdomyolysis
- Treament and anesthetic management of rhabdomyolysis
Definition and mechanisms
- Rhabdomyolysis occurs when damaged skeletal muscle breaks down rapidly and releases its content in the bloodstream
- Characterized by skeletal muscle disintegration and the release of myoglobin and other intercellular proteins and electrolytes into the circulation
- Hyperkalemia, hyperuricemia, and hyperphosphatemia can all develop rapidly
- This can lead to heart- or kidney failure and can even be fatal
- Rhabdomyolysis ranges from an asymptomatic illness with elevation in the CK level to a life-threatening condition associated with extreme elevations in CK, electrolyte imbalances, acute kidney injury, and disseminated intravascular coagulation
- Most often caused by direct traumatic injury, however, can also result from a wide array of other causes
Signs and symptoms
- Muscle pains or cramps
- Weakness
- Swelling of affected muscles
- Nausea and vomiting
- Confusion
- Coma
- Tea-colored urine due to the presence of myoglobin
- Abdominal pain
- Fever
- Tachycardia
- Arrhythmias
- Hypotension and shock
- Acute kidney injury
AKI and rhabdomyolysis
- Myoglobin interacts with the Tamm-Horsfall protein in the renal tubules to form brown granular casts which lead to tubular obstruction
- This process is favoured when the urine is acidic
- The heme group of myoglobin could lead to lipid peroxidation
- Myoglobin also scavenges nitrous oxide leading to renal vasoconstriction
- Renal blood flow is furter reduced by hypovolemia, activation of the RAAS system and other vascular mediators
Complications
- Hyperkalemia
- Hypocalcemia
- Acute kidney injury
- Disseminated intravascular coagulation
- Compartment syndrome
Causes
- Strenuous exercise
- Delirium tremens
- Tetanus
- Prolonged seizures
- Crush injuries
- Arterial thrombosis or embolism
- Clamping of an artery during surgery
- Hyperthermia
- Hypothermia
- Drugs and toxins
- Statins and fibrates
- Antipsychotic medications may cause the neuroleptic malignant syndrome
- Neuromuscular blocking agents used in anesthesia may result in malignant hyperthermia, also associated with rhabdomyolysis
- Medications that cause serotonin syndrome, such as SSRIs
- Medications that interfere with potassium levels, such as diuretics
- Heavy metals
- Venom from insects or snakes
- Drugs: alcohol, amphetamine, cocaine, heroin, ketamine, and MDMA
- Infection
- Electrical injury
- Immobilization
- Metabolism:
- Hyperglycemic hyperosmolar state
- Hyper– and hyponatremiamia
- Hypokalemia
- Hypocalcemia
- Hypophosphatemia
- Ketoacidosis
- Hypothyroidism
Risk factors
| Endogenous Risks | Exogenous Risks |
|---|---|
| Advanced age (> 80 years) Small body frame and frailty Multisystem disease - Renal dysfunction - Hepatic dysfunction Thyroid disorders, especially Hypothyroidism Hypertriglyceridemia Metabolic muscle disease - Carnitine palmitoyltransferase II deficiency - McArdle disease Myoadenylate deaminase deficiency | Alcohol consumption Heavy exercise Surgery with severe metabolic demands Agents affecting the cytochrome P450 system, especially - Fibrates - Nicotinic acid - Cyclosporine - Azole antifungals - Macrolide antibiotics - HIV protease inhibitors - Nefazodone - Verapamil - Amiodarone - Warfarin - Consumption of > 1 quart daily of grapefruit juice |
Diagnosis
- Blood test: creatine kinase (CK) > 5000 U/L
- Note that myoglobin levels peak before increases in CK
- However, myoglobin is metabolized rapidly at sites outside of the kidney
- This makes CK a more reliable marker of rhabdomyolysis
| Investigations | Possible findings |
|---|---|
| Serum and urine myoglobin | Present |
| Urinary dipstick + pH | Positive for blood |
| Urea and creatinine | Raised |
| Potassium | Raised |
| Calcium | Low |
| Phosphate, uric acid | Raised |
| Coagulation studies | Prologend in severe cases |
| Blood gas | Lactic acidosis |
| Calculation of anion gap | Raised |
| ECG | Prologend in severe cases |
- A metabolic acidosis with a high anion gap is commonly reported in rhabdomyolysis with associated AKI
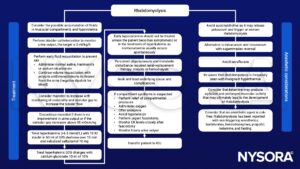
Management
Suggested reading
- Floridis, J., Barbour, R., 2022. Postoperative weakness and anesthetic-associated rhabdomyolysis in a pediatric patient: a case report and review of the literature. Journal of Medical Case Reports 16.
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Torres PA, Helmstetter JA, Kaye AM, Kaye AD. Rhabdomyolysis: pathogenesis, diagnosis, and treatment. Ochsner J. 2015;15(1):58-69.
- Williams J, Thrope C. 2014. Rhabdomyolysis. Continuing Education in Anaesthesia Critical Care & Pain. 14;4:163-166.
- Hunter JD, Greggg K, Damani S. 2006. Rhabdomyolysis. Continuing Education in Anaesthesia Critical Care. 6;4:141-143.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com