Learning objectives
- Recognize the different classes of cardiomyopathies
- Anesthetic management of patients with cardiomyopathy
Definition & mechanisms
- Cardiomyopathy is myocardial disorder in which the heart muscle is structurally and functionally abnormal
- Can be inherited or acquired
- Can affect all age groups
- Affects the shape, function, and electrical system of the heart.
- Signs and symptoms can usually be managed successfully and patients can have a good life expectancy
Dilated cardiomyopathy
- Dilatation of the left and right ventricles, impaired systolic function
- Major cause of heart failure and arrhythmia in young adults
- Two-thirds of cases are idiopathic
- Possible causes:
- Familial association
- Post-viral infection
- Part of a disease process (ischemic heart disease, hypertension, diabetes, malformation syndrome, alcohol excess, neuromuscular disorder, inborn errors of metabolism, exposure to cardiotoxic agents)
- Asymptomatic in early stages
- Symptoms of heart failure (dyspnea, fatigue, ascites, peripheral edema, arrhythmias)
- Embolic events and sudden death may occur at a later stage
- Diagnosis: Echocardiography, chest radiograph, electrocardiography, blood tests, detailed medical and family history, physical examination
Management
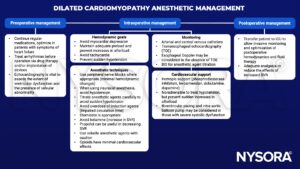
SVR, systemic vascular resistance; BIS, bispectral index; ICU, intensive care unit
Hypertrophic cardiomyopathy
- Hypertrophy of the left ventricle in the absence of other structural or functional abnormalities
- Inherited disease of the myocardium
- Hypertrophy can be asymmetrical, concentric, midventricular, apical, and can also involve the right ventricle
- Diastolic impairment of the left ventricle
- End-stage: Biventricular systolic dysfunction due to myocardial fibrosis
- 70% of cases have obstructive hypertrophy
- Majority of patients is asymptomatic
- Symptoms of angina and heart failure (dyspnea, chest pain, syncope, arrhythmia)
- Severe complications: Angina pectoris, heart failure, sudden death
Management
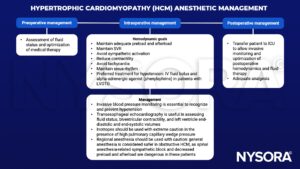
SVR, systemic vascular resistance; LVOTO, left ventricular outflow tract obstruction
Restrictive cardiomyopathy
- Impairment of ventricular diastolic function due to fibrotic or infiltrative changes in the myocardium and/or subendocardium
- Primary or secondary (amyloidosis, sarcoidosis, hemochromatosis, ischemic heart disease, hypertension, valvular disease)
- Symptoms of biventricular failure (dyspnoea, orthopnea, fatigue, palpitation, edema, chest pain)
- On physical examination, patients may have an audible third heart sound, systolic murmur, raised jugular venous pressure, ascites, and peripheral edema
- Diagnosis: Echocardiography, endomyocardial biopsy, computed tomography, cardiac MRI
Management
- General anesthesia causes vasodilation, suppresses the myocardium, and reduces venous return. The latter can be exacerbated by intermittent positive ventilation resulting in cardiac arrest.
- Invasive arterial blood pressure monitoring and transesophageal echocardiography are useful in identifying the causes of cardiovascular instability.
- Hemodynamic goals:
- Maintain adequate preload, SVR, and sinus rhythm
- Use an anesthetic agent with minimal cardiovascular effect (ketamine or etomidate)
Arrhythmogenic right ventricle cardiomyopathy
- Structural abnormalities and cardiac dysfunction of the right ventricle, can also involve left ventricle
- Complex genetic condition
- Other causes: Degenerative disease, infection, inflammation
- Usually starts as a localized disease with regional wall abnormalities
- Development of right bundle branch block followed by right ventricular failure between the fourth and fifth decades of life
- Young patients often present with arrhythmia, syncope, cardiac arrest, or sudden death
- 3 clinical phases:
- Phase 1 (concealed disease): Some structural abnormality in the myocardium, patients can present with sudden cardiac death
- Phase 2 (overt disease): Established structural abnormality of the myocardium, patients present with arrhythmias and syncope
- Phase 3 (End-stage disease): Severe structural changes
Management
- Arrhythmias of both supraventricular and ventricular may occur at any time
- Avoid hypovolemia, hypercarbia, acidosis and lighter depth of anesthesia
- Amiodarone is the first line of medication to treat rhythm disturbances
- Placement of implantable cardioverter defibrillator is beneficial
Suggested reading
- Ibrahim IR, Sharma V. Cardiomyopathy and anaesthesia. BJA Education. 2017;17(11):363-9.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com