Learning objectives
- Describe the risk factors for malignant hyperthermia
- Describe the symptoms of malignant hyperthermia
- Manage malignant hyperthermia and its consequences
Definition & mechanism
- Malignant hyperthermia (MH) is caused by genetic defects, most commonly in the RYR1 gene (more rarely affected genes include CACNA1S and STAC3)
- Caused by an increase in metabolic rate driven by an increase in intracellular calcium levels in muscle tissue
- Can be triggered when exposed to potent inhalation anesthetics and/or succinylcholine
Risk factors
Patients that have a higher risk of MH when exposed to triggering agents:
- Any close relative has a confirmed susceptibility to MH
- The patient or a close relative has a history of an event that is suspected to be MH during anesthesia
- The patient or a close relative has a history of rhabdomyolysis, which can be triggered by exercise in extreme heat and humidity or when taking a statin drug
- Patients with another genetic muscle disorder (e.g. Duchenne muscular dystrophy)
- Patients with idiopathic hyperCKemia
- Patients with otherwise unexplained exertional heat illness
Symptoms
- Unexplained, unexpected increase in ETCO2
- Unexplained, unexpected increase in heart rate
- Unexplained, unexpected increase in temperature
- Decreased urine output
- Muscle spasms
- Masseter muscle rigidity
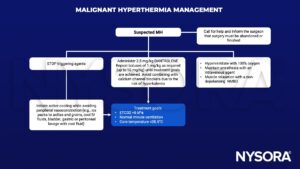
Management
Supportive management
- Hyperkalemia may require administration of calcium chloride, sodium bicarbonate, and/ or insulin with glucose
- Treat arrhythmias with magnesium, amiodarone or beta-blockers. Avoid calcium channel blockers as they interact with dantrolene, potentiating myocardial depression
- Disseminated intravascular coagulation may require blood product transfusion
- Rhabdomyolysis may result in acute kidney injury; measure creatine kinase and institute forced alkaline diuresis
- Transfer the patient to the ICU once sufficiently stable
Follow-up:
- The diagnosis of MH is confirmed by muscle biopsy and in vivo contracture testing at specialist centers
- The patient and their family members must be followed-up and counseled regarding future anesthetics
- An alert should be documented in the patient notes and the patient should consider wearing an alert bracelet or carrying an alert card to notify medical staff of their condition in case of future emergencies
Keep in mind
- Taking a personal and family history of anesthetic problems is a mandatory part of the preoperative assessment for all patients requiring general or regional anesthesia
- Activated charcoal filters should be available at all anesthetizing locations
- Patients at increased risk of developing malignant hyperthermia must not be exposed to potent inhalation anesthetics or succinylcholine
Suggested reading
- Hopkins PM, Girard T, Dalay S, et al. Malignant hyperthermia 2020: Guideline from the Association of Anaesthetists. Anaesthesia. 2021;76(5):655-664.
- Gupta, Pawan K, and Philip M Hopkins. “Diagnosis and Management of Malignant Hyperthermia.” BJA Education, vol. 17, no. 7, July 2017, pp. 249–254, 10.1093/bjaed/mkw079.
We would love to hear from you. If you should detect any errors, email us at [email protected]