Learning objectives
- Describe the mechanisms and risk factors for venous thromboembolism
- Prevent perioperative venous thromboembolism
- Diagnose and manage venous thromboembolism
Background
- Venous thromboembolism (VTE) is a major cause of morbidity and mortality in both hospital and community settings
- Most preventable cause of mortality in hospitalized patients
- Encompasses deep vein thrombosis (DVT) and pulmonary embolism (PE)
- DVT occurs when red blood cells, fibrin, platelets, and leucocytes form a mass within an intact deep vein
- Signs & symptoms are nonspecific and only occur in up to 50% of patients
- PE occurs in about a third of patients with a DVT
- Adequate perioperative thromboprophylaxis is essential to prevent perioperative VTE
Risk factors
- Three main factors that cause thrombosis:
- Alterations in blood flow (stasis and turbulence)
- Vascular endothelial injury
- Alterations in the blood coagulability
- Risk factors:
| Stasis–endothelial injury | Thrombophilias | Medical conditions | Medications | Other |
|---|---|---|---|---|
| Indwelling venous device | Activated protein C resistance | Malignancy (solid tumour and myeloproliferative disorders) | Oral contraceptive use (combined only) | Increasing age |
| Surgery (abdominal, pelvic, orthopedic most commonly) | Factor V Leiden | Pregnancy, postpartum | Hormone replacement therapy | Smoking |
| Major trauma, burns | Prothrombin gene mutation G20210A | Myocardial infarction | Chemotherapy (including tamoxifen) | |
| Prolonged travel | Hyperhomocysteinemia | Congestive heart failure | ||
| Paralysis (including anesthesia for >30 min) | Anticardiolipin antibodies | Obesity | ||
| Varicose veins | Lupus anticoagulant | Inflammatory bowel disease | ||
| Elevated factor VIII level | Nephrotic syndrome | |||
| Protein C deficiency | History of VTE | |||
| Protein S deficiency | Heparin-induced thrombocytopenia | |||
| Dysfibrinogenemia | Paroxysmal nocturnal hemoglobinuria | |||
| Dysplasminogenemia | ||||
| Antithrombin deficiency |
Pathophysiology
- Venous thrombi typically develop at a site of vascular trauma, around intravascular catheters, or in areas of reduced blood flow (e.g., venous valves)
- Accumulation of fibrin and platelets causes rapid growth in the direction of blood flow
- Endogenous fibrinolysis results in partial or complete resolution of the thrombus
- Any residual thrombus may result in incomplete recanalization of the vein, potentially narrowing the lumen and causing valve incompetence
- Extensive collateral network may develop
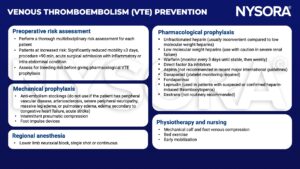
Prevention
Diagnosis
- DVT
- Duplex ultrasonography
- D-dimer blood test
- Contrast venography
- MRI
- PE
- Computed tomographic pulmonary angiography
- Ventilation-perfusion scan
- Pulmonary angiography
- MRI
Management
- Preferred DVT treatment: Low molecular weight heparins
- Maintain anticoagulation for 3-6 months for VTE secondary to transient risk factors and >12 months for recurrent VTE
- Thrombolytics in severe cases
- When anticoagulation fails: Inferior vena cava filter
- Thrombectomy/embolectomy (rarely required)
Suggested reading
- Gordon RJ, Lombard FW. Perioperative Venous Thromboembolism: A Review. Anesthesia & Analgesia. 2017;125(2).
- Barker RC, Marval P. Venous thromboembolism: risks and prevention. Continuing Education in Anaesthesia Critical Care & Pain. 2011;11(1):18-23.
- National Clinical Guideline Centre – Acute and Chronic Conditions (UK). Venous Thromboembolism: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital. London: Royal College of Physicians (UK); 2010. (NICE Clinical Guidelines, No. 92.) 2, Summary of recommendations. Available from: https://www.ncbi.nlm.nih.gov/books/NBK116536/
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com