Learning objectives
- Describe the etiology and symptoms of hypothyroidism
- Diagnose and treat hypothyroidism
- Manage patients with hypothyroidism presenting for surgery
Background
- Hypothyroidism results from low levels of thyroid hormone
- Autoimmune thyroid disease and lack of dietary iodine are the most common causes
- Can range from asymptomatic to myxedema coma
- Can be treated with exogenous thyroid hormone
Etiology
- Primary hypothyroidism: The thyroid gland does not produce adequate amounts of thyroid hormone
- Iodine deficiency
- Autoimmune (Hashimoto thyroiditis)
- Medications (amiodarone, thalidomide, oral tyrosine kinase inhibitors, stavudine, interferon, bexarotene, perchlorate, rifampin, ethionamide, phenobarbital, phenytoin, carbamazepine, interleukin-2, lithium)
- Thyroid radioactive iodine therapy
- Thyroid surgery
- Radiotherapy to head or neck area
- subacute granulomatous thyroiditis
- Postpartum thyroiditis
- Secondary hypothyroidism: Thyroid gland is normal, pathology is related to pituitary gland or hypothalamus
- Neoplastic, infiltrative, inflammatory, genetic, or iatrogenic disorders of the pituitary or hypothalamus
- Sheehan syndrome
- Thyrotropin-releasing hormone (TRH) resistance
- TRH deficiency
- Lymphocytic hypophysitis
- Radiation therapy to the brain
- Medications such as dopamine, prednisone, or opioids
Risk factors
- Women >60 years of age
- Pregnancy
- History of head and neck irradiation
- Autoimmune disorders
- Type I diabetes mellitus
- Positive thyroid peroxidase antibodies
- Family history of hypothyroidism
Signs & symptoms
- Cold intolerance
- Puffiness
- Decreased sweating
- Dry skin
- Hair loss
- Constipation
- Fatigue
- Muscle cramps
- Sleep disturbance
- Menstrual cycle abnormalities
- Weight gain
- Galactorrhea
- Depression
- Anxiety
- Psychosis
- Cognitive impairments
- Carpal tunnel syndrome
- Sleep apnea
- Hyponatremia
- Hypercholesterolemia
- Congestive heart failure
- Prolonged QT interval
- Fullness of throat
- Painless thyroid enlargement
- Episodic neck pain/sore throat
- Pallor and jaundice
- Dull facial expressions
- Macroglossia
- Bradycardia
- Pericardial effusion
- Prolonged ankle reflex relaxation time
Diagnosis
- Serum thyroid stimulating hormone (TSH) level to test for primary hypothyroidism
- Serum-free T4 level to test for secondary hypothyroidism
- Serum anti-thyroid antibodies to test for autoimmune thyroid disease
- Other laboratory tests may reveal hyperlipidemia, elevated serum CK, elevated hepatic enzymes, anemia, blood urea nitrogen, creatinine, and uric acid levels
Differential diagnosis
- Euthyroid sick syndrome
- Goiter
- Myxedema coma
- Anemia
- Riedel thyroiditis
- Subacute thyroiditis
- Thyroid lymphoma
- Iodine deficiency
- Addison disease
- Chronic fatigue syndrome
- Depression
- Dysmenorrhea
- Erectile dysfunction
- Familial hypercholesterolemia
- Infertility
Treatment
- Main treatment: levothyroxine monotherapy 1.6 µg/kg per day
- Lower the dose in elderly and atrial fibrillation patients
- IV levothyroxine in patients who cannot take it orally (half of the oral dose)
- Treat adrenal insufficiency first
Anesthetic management
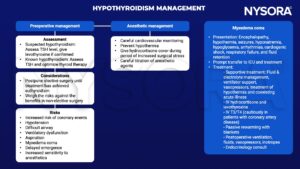
TSH, thyroid stimulating hormone; T3, triiodothyronine; T4, thyroxine
Suggested reading
- Patil N, Rehman A, Jialal I. Hypothyroidism. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519536/
- Farling PA. Thyroid disease. BJA: British Journal of Anaesthesia. 2000;85(1):15-28.
- Palace MR. Perioperative Management of Thyroid Dysfunction. Health Serv Insights. 2017;10:1178632916689677. Published 2017 Feb 20.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com