Learning objectives
- Define and classify arrhythmias
- Describe the patient, anesthetic, and surgical risk factors for developing intraoperative arrhythmias
- Management of intraoperative arrhythmias
Definition and mechanisms
- Arrhythmias are accelerated, slowed, or irregular heartbeats caused by abnormalities in the electrical impulses of the myocardium
- 60% of patients may experience perioperative arrhythmias
- The majority are benign, but rhythm disturbance can be associated with potentially serious adverse outcomes
Classification
Bradyarrhythmia (HR <60 bpm)
- Sinus arrhythmia: Sinus bradycardia
- Conduction defects
- AV blocks
- First-degree AV block
- Second-degree AV block
- Third-degree AV block
- Intraventricular blocks
- Right bundle branch block
- Left bundle branch block
- Fascicular block
- Left anterior hemiblock
- Right anterior hemiblock
- Bifascicular block
- Trifascicular block
- AV blocks
Tachyarrhythmia (HR >100 bpm)
- Sinus arrhythmia: Sinus tachycardia
- Supraventricular arrhythmias
- Premature atrial contraction
- Supraventricular tachycardia
- Atrial flutter
- Atrial fibrillation
- Ventricular arrhythmias
- Premature ventricular contractions
- Ventricular tachycardia
- Ventricular fibrillation
- Torsade de pointes
Complications
- Blood clots (i.e., thromboembolism)
- Stroke
- Heart failure
- Sudden death
Risk factors
Patient factors
- Preexisting arrhythmias
- Coronary artery disease
- Hypertension
- Congestive heart failure
- Electrolyte disorders (especially potassium, magnesium, and calcium)
- Valvular heart disease
- Obstructive sleep apnea
- Medications:
- β2-agonists
- Theophylline
- Tricyclic antidepressants
- Less common causes:
-
- Thyroid disease (i.e., hypothyroidism, hyperthyroidism)
- Cardiomyopathies (including alcoholic)
- Myocarditis
- Trauma (myocardial or intracranial)
- Connective tissue disorders
- Smoking
- Drug and solvent abuse
Anesthetic factors
- Hypotension or hypertension (e.g., inadequate anesthesia)
- Hypoxia
- Hypercarbia
- Direct laryngoscopy and intubation
- Central nervous pressure lines (irritation by line tip; microshock hazard)
- Drugs
- Volatile anesthetic agents
- Local anesthetics
- Suxamethonium
- Pancuronium
- Multiple drugs prolong the QT interval (e.g., volatile agents, macrolide antibiotics, butyrophenone antipsychotics, amiodarone, and ondansetron)
- 4Hs 4Ts
- Hypovolemia, hypoxemia, hyper/hypokalemia (electrolyte disorders) and metabolic disorders (acidosis), and hypo/hyperthermia
- Tension pneumothorax, tamponade, toxins/drugs, thromboembolism (pulmonary/cardiac)
Surgical factors
- Catecholamines
- Endogenous (from any surgical stimulus)
- Exogenous (topical or infiltrated epinephrine)
- Autonomic stimulation
- Peritoneal and visceral traction
- Peritoneal insufflation
- Trigeminovagal reflexes (oculocardiac reflex)
- Laryngoscopy, bronchoscopy, esophagoscopy
- Carotid artery and thyroid surgery
- Direct stimulation of the heart during cardiac or thoracic surgery
- Embolism
- Thrombus
- Fat
- Bone cement
- Air
- Carbon dioxide
- Amniotic fluid
- Other
- Aortic cross-clamping
- Limb reperfusion
- Glycine intoxication
Treatment goals
- Prevent thromboembolism formation
- Control heart rate
- Correct the condition causing the arrhythmia
- Reduce other risk factors for heart disease and stroke
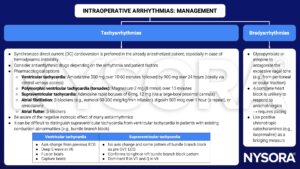
Management
- More than one factor is likely to contribute to the development of an intraoperative arrhythmia
- Identify the rhythm
- Evaluate its significance (in the context of)
- Coexisting medical problems and their treatment
- Surgical condition
- Operative procedure
- Anesthetic drugs and technique
- Hemodynamic effect of the arrhythmia and the risk of progression to a more serious arrhythmia
- Identify and correct any precipitating factors
- Take an ABC approach
- Treat the whole patient, not just the ECG
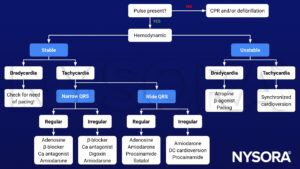
Algorithm
Prevention
- Keep surgical manipulations that can precipitate arrhythmias to a minimum
- An adequate depth of anesthesia may prevent or control intraoperative arrhythmias
- Prevent hypoxia, hypotension, hypovolemia, and hypothermia during surgery
Suggested reading
- Noor ZM. Md. Life-Threatening Cardiac Arrhythmias during Anesthesia and Surgery. Cardiac Arrhythmias – Translational Approach from Pathophysiology to Advanced Care. 2021. doi: 10.5772/intechopen.101371.
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 30 Management problems, Shelton C.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







