Explore NYSORA knowledge base for free:

New York City—where tradition meets tomorrow—is setting the stage for an electrifying convergence of minds and ideas. In the heart of Times Square, NYSORA is redefining the art and science of anesthesia with an event that’s as innovative as it is international. What’s On the Program? Master the Complex: Tackle high-risk cases, from obesity and OSA challenges to breakthrough orthopedic procedures. Stay on the Cutting Edge: Dive into the latest in opioid-free anesthesia, fluid resuscitation breakthroughs, and revolutionary high-flow nasal cannula techniques. Embrace the Future: See firsthand how AI, machine learning, and advanced ultrasound techniques are reshaping anesthetic safety and efficiency. Champion Wellness & Sustainability: Explore strategies to shrink anesthesia’s carbon footprint, fight burnout with biohacking, and discover pioneering approaches to pain management and longevity. Elevate Your Expertise: Gain hands-on experience with advanced nerve block techniques, spinal anesthesia innovations, and more—bringing transformative skills back home. At its 18th edition, the NYSORA Symposium isn’t just an event—it’s the birthplace of the future of anesthesiology. Join us at the Sheraton in Times Square from September 26-28, 2025. Secure your spot now and be part of the revolution in anesthesia. Who else but NYSORA calls NYC home? Register Today.

Total hip arthroplasty (THA) is a frequently performed surgical procedure to improve mobility and quality of life in patients with advanced hip joint disease. However, significant postoperative pain is a common challenge and can hinder recovery, delay rehabilitation, and increase opioid consumption. Multimodal analgesia, incorporating a combination of systemic and regional techniques, has become the cornerstone of postoperative pain management in THA. The anterior quadratus lumborum block (QLB) has emerged as a potential technique for addressing the complex innervation of the hip joint. This multicenter, randomized, placebo-controlled trial evaluated whether adding anterior QLB to multimodal analgesia improves postoperative outcomes in patients undergoing THA. Study objective and methods The study aimed to assess the impact of anterior QLB on postoperative pain, opioid consumption, and functional recovery in THA patients. Design: Multicenter, randomized, double-blind, placebo-controlled trial. Participants: 60 patients undergoing primary unilateral THA were randomized to receive either anterior QLB with 20 mL of 0.2% ropivacaine (n = 30) or a placebo saline injection (n = 30). Intervention: Anterior QLB was performed preoperatively with ultrasound guidance, injecting local anesthetic or saline between the quadratus lumborum and psoas major muscles. Both groups received multimodal analgesia, including NSAIDs, acetaminophen, ketamine, and dexamethasone. Primary outcome: Cumulative opioid consumption (oral morphine equivalents) in the first 24 hours postoperatively. Secondary outcomes: Pain scores, time to first standing, walking distance, quadriceps strength, and 3-month functional recovery metrics. Key findings Opioid consumption: There was no significant difference in cumulative opioid consumption between the QLB and placebo groups. Median opioid use in the first 24 hours was 40 mg (IQR 20–50 mg) for the QLB group and 31 mg (IQR 20–45 mg) for the placebo group (P = 0.6). Pain scores: Pain intensity was similar between the two groups at all measured time points. The QLB group did not […]
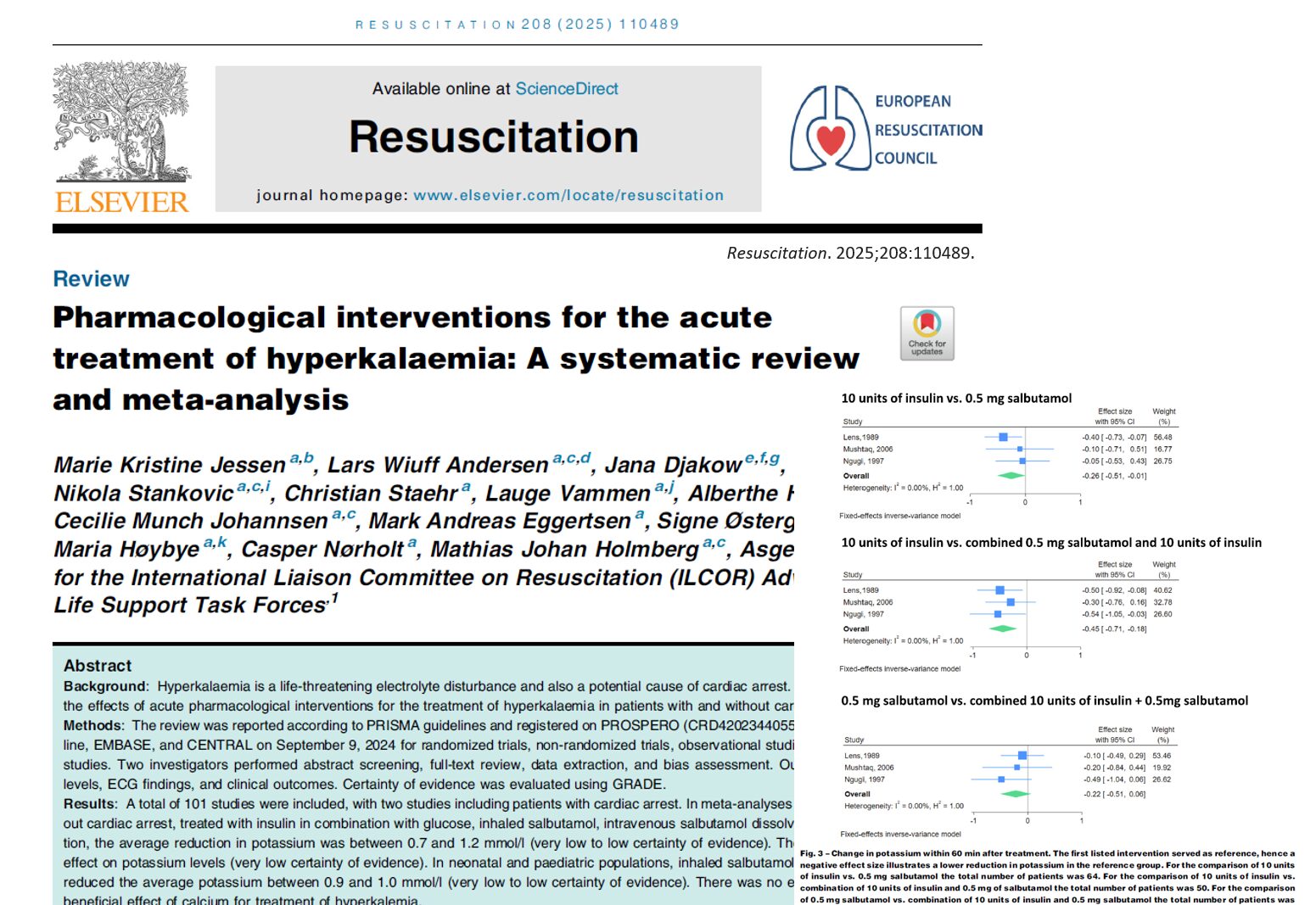
Hyperkalemia, a potentially fatal electrolyte disorder characterized by elevated serum potassium levels, remains a significant challenge in clinical practice. A newly published systematic review and meta-analysis (Jessen et al., 2025) has now meticulously examined the efficacy of various pharmacological interventions in treating acute hyperkalemia, including cases with and without cardiac arrest. The results provide crucial insights into optimal treatment strategies, raising questions about some long-standing clinical practices. What is Hyperkalemia? Definition: Adults: Serum potassium ≥ 6.5 mmol/L (Severe Hyperkalemia) Neonates/Premature neonates: Serum potassium ≥ 6.0–6.5 mmol/L Normal range: 3.5 – 5.0 mmol/L Risks: Severe hyperkalemia may cause life-threatening arrhythmias and sudden cardiac death. Effective pharmacological interventions 1. Insulin with Glucose/Dextrose Mechanism: Facilitates transcellular shift of potassium into cells. Adult population: 10 units insulin + glucose reduced potassium by 0.7 – 1.4 mmol/L within 60 minutes. Meta-analysis result: Average potassium reduction of 0.7 mmol/L. Neonatal/Pediatric population: Weight-based approaches showed variable results. 2. Beta2-Agonists (Salbutamol/Albuterol) Inhaled Salbutamol: Adults: Doses: 10–20 mg inhaled Potassium reduction: −0.9 mmol/L Neonates/Pediatrics: 400 mcg of inhaled salbutamol reduced potassium by −0.9 mmol/L. Intravenous Salbutamol: Adults: 0.5 mg IV salbutamol (dissolved in glucose): −1.0 mmol/L potassium reduction. Combining IV salbutamol with insulin + glucose resulted in −1.2 mmol/L reduction. Neonates/Pediatrics: 4–5 mcg/kg IV salbutamol reduced potassium by −1.0 mmol/L. 3. Combination therapies Insulin + IV Salbutamol (0.5 mg) + Glucose: Superior to insulin alone. Potassium reduction: Up to −1.2 mmol/L within 60 minutes. Ineffective or uncertain interventions 1. Bicarbonate Five adult studies showed no significant potassium reduction (mean change: −0.1 mmol/L). 2. Calcium (Calcium Chloride/Gluconate) No evidence supporting clinical benefit in hyperkalemia management. Some observational studies suggest possible worse outcomes during cardiac arrest, but results have a high risk of bias. Traditionally used to stabilize myocardial cells but lacks concrete evidence for improving survival outcomes. Acute management of […]