Learning objectives
- Identify the causes leading to delayed emergence
- Explain the risk factors associated with an increased risk of delayed emergence
- Manage delayed emergence
Definition and mechanism
- Failure to regain consciousness or alertness following general anesthesia after surgery
- The transition from unconsciousness to complete wakefulness occurs along a normal trajectory, although slowed down
- Alternatively, the awakening trajectory proceeds abnormally, possibly leading to emergence delirium
- Most cases of delayed return of consciousness are rapidly treatable
Causes
| Pharmacodynamic causes | Genetic variations Hypothermia Drug interaction Serotonin syndrome Neuromuscular blockers Heroin or opioid toxicity IV anesthetic agents (Total intravenous anesthesia (TIVA)) Central anticholinergic syndrome |
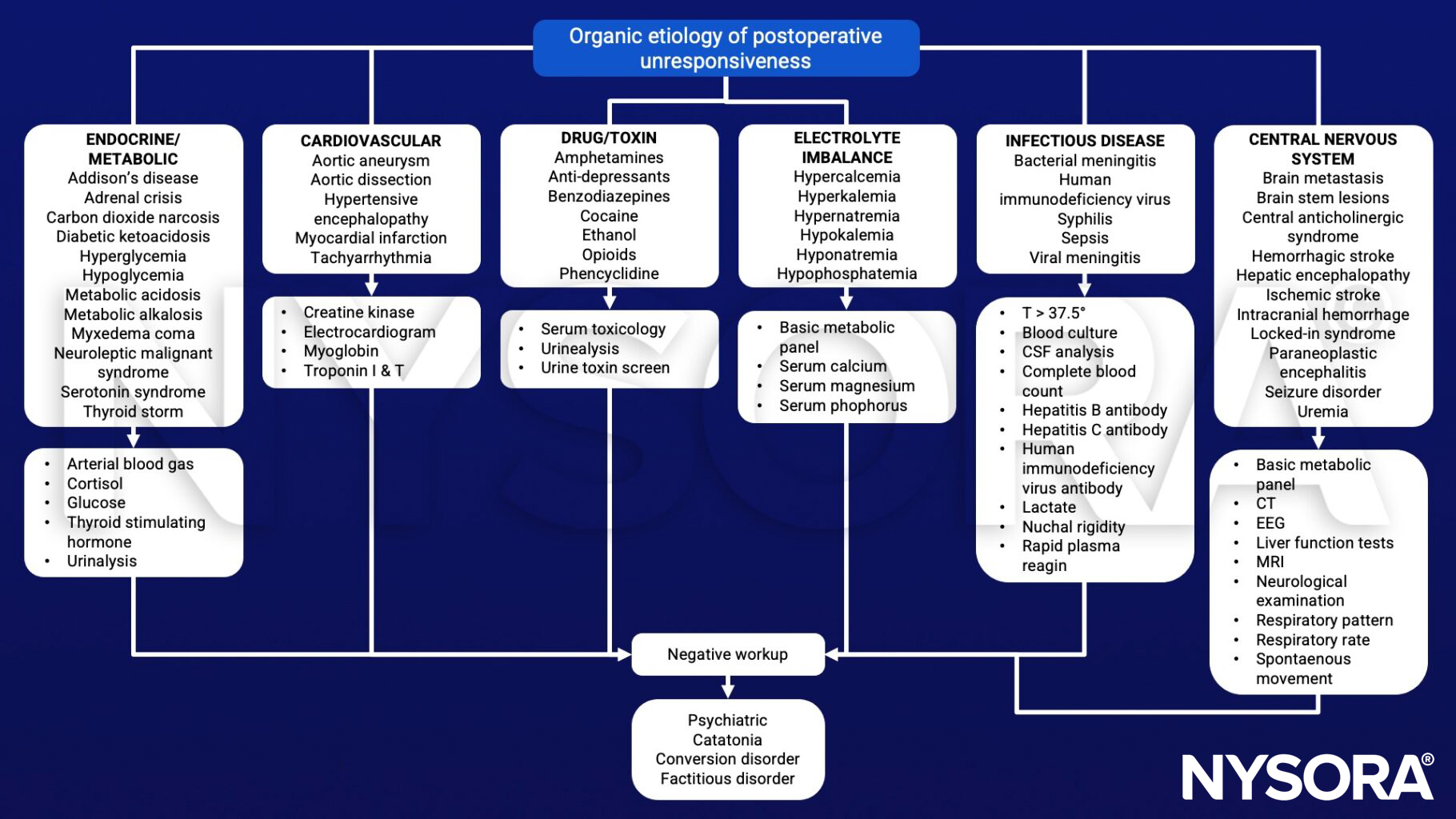
| Metabolic alterations | Hypoglycemia Hyperglycemia Hyponatremia Hypernatremia Metabolic acidosis |
| Neurological rare causes | Hypoperfusion/ischemia Intracranial hemorrhage Venous thromboembolism Seizures Myxedema coma Functional coma Brainstem stroke |
| Psychiatric rare causes | Conversion disorder |
Risk factors
| Patients conditions | Older age Body habitus Gender | |
| Preexisting clinical conditions | Psychological disorders Neurologic conditions Cardiac diseases Hypertension Pulmonary diseases Chronic kidney disease Liver diseases Hypothyroidism Drug or alcohol abuse Metabolic alterations | |
| Intraoperative conditions | Drugs (e.g. Heroin or opioid toxicity) Metabolic alterations (intraoperative) | |
| Chronic pharmacotherapy | Benzodiazepines Barbiturates Anticholinergics Antidepressants Antipsychotics Herbal medications |
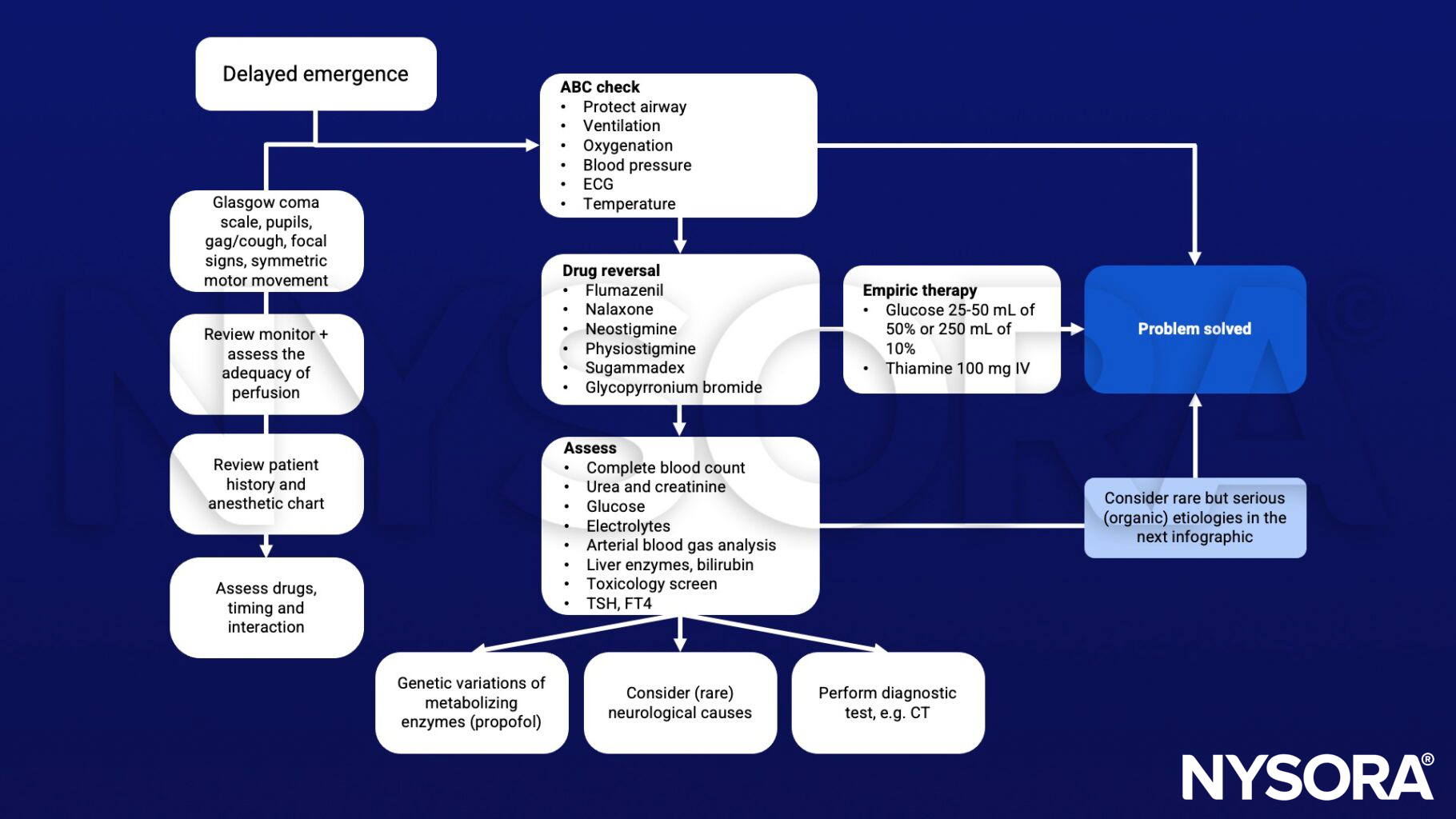
Diagnostic steps
- Vital signs (including temperature)
- neuromuscular monitor
- Neurologic exam (pupils, cranial nerves, reflexes, response to pain)
- Fingerstick glucose
- Arterial blood gas with electrolytes
Differential diagnosis
| Drug effects | Residual anesthetic (volatile, propofol, barbiturates, ketamine) Excess narcotics Inadequate reversal or no reversal of muscle relaxation Pseudocholinesterase deficiency Alcohol or street drugs Herbal medicines (valerian root, St. John’s wort) Infection |
| Infection | Encephalitis Meningitis Sepsis |
| Metabolic disorders | Hypercarbia Hypoxemia Metabolic acidosis Acidosis Hypoglycemia/Hyperglycemia Hyponatremia/electrolyte abnormalities Hypothermia/Malignant hyperthermia Uremia Hepatic encephalopathy Osmolality problems Myxedema coma |
| Neurologic disorders | New ischemic event Subarachnoid hemorrhage Seizures or postictal state Increased intracranial pressure or pre-existing obtundation Perioperative stroke (ischemic or hemorrhagic) Hydrocephalus Diffuse anoxic injury Pneumocephalus Cerebral hyperperfusion syndrome |
Management
Additional facts
- Recent studies indicate that induction and awakening are asymmetric processes
- Neural circuits that mediate induction do not completely overlap those that mediate emergence for anesthesia
Suggested reading
- Cascella M, Bimonte S, Di Napoli R. Delayed Emergence from Anesthesia: What We Know and How We Act. Local Reg Anesth. 2020 Nov 5;13:195-206.
- Thomas E, Martin F, Pollard B. Delayed recovery of consciousness after general anaesthesia. BJA Educ. 2020 May;20(5):173-179.
- Rafizadeh S, Kerry-Gnazzo AR, DeWalt K. An Unresponsive Patient in Postanesthesia Care Unit: A Case Report of an Unusual Diagnosis for a Common Problem. A A Pract. 2020 Aug;14(10):e01293.
- Yonekura H, Murayama N, Yamazaki H, Sobue K. A Case of Delayed Emergence After Propofol Anesthesia: Genetic Analysis. A A Case Rep. 2016 Dec 1;7(11):243-246.
Clinical updates
Vetter et al. (European Journal of Anaesthesiology, 2025) report in a single-center RCT of carotid endarterectomy patients that co-administration of dexmedetomidine with TIVA reduced propofol effect-site concentrations required for burst suppression by 33% and decreased vasopressor requirements by 50%, without impairing neurophysiologic monitoring. Importantly, dexmedetomidine did not increase delayed emergence, with comparable postoperative GCS scores and no difference in delirium rates between groups. These findings suggest that dexmedetomidine’s propofol-sparing effect may enhance hemodynamic stability without prolonging recovery, supporting its integration into high-risk neurovascular anesthesia protocols.
- Read more about this study HERE.