Learning objectives
- Describe the physiology, causes, and effects of metabolic acidosis
- Diagnose metabolic acidosis
- Manage metabolic acidosis
Background
- Metabolic acidosis is a disturbance in the homeostasis of plasma acidity
- Any process that increases the serum hydrogen ion concentration is a distinct acidosis
- A patient can have multiple acidoses contributing to the decrease of serum pH
- Adicosis can be either respiratory (changes in CO2) or metabolic (changes in bicarbonate)
- Metabolic acidosis is characterized by an increase in serum hydrogen ion concentration resulting in serum bicarbonate (HCO3) <24 mEq/L
- May be associated with organ failure, especially respiratory and cardiovascular
- Can be acute or chronic
Etiology
- Classification of metabolic acidosis is based on the presence or absence of an anion gap (concentration of unmeasured serum anions)
- Sodium, the main plasma cation, is balanced by the sum of the anions bicarbonate and chloride in addition to the unmeasured anions (e.g., lactate, acetoacetate), which represent the anion gap
- Anion gap metabolic acidosis is often caused by anaerobic metabolism and lactic acid accumulation
- Non-gap metabolic acidosis is primarily caused by the loss of bicarbonate (e.g., diarrhea, renal tubular acidosis)
- Causes:
| Anion gap metabolic acidosis | Non-gap metabolic acidosis associated with normal or high serum K+ | Non-gap metabolic acidosis associated with low serum K+ |
|---|---|---|
| Acute kidney injury | Administration of HCl or precursors | Diarrhea |
| Chronic kidney disease | Administration of cationic amino acids | intestinal, pancreatic, or biliary fistula |
| Diabetic ketoacidosis | Chronic kidney disease | Proximal renal tubular acidosis |
| Alcoholic ketoacidosis | Adrenal insufficiency (primary or secondary) | Distal renal tubular acidosis |
| Lactic acidosis | Hyporeninemic hypoaldosteronism | Ureterosigmoidostomy |
| Salicylate intoxication | Hyperkalemic distal renal tubular acidosis | Ureteroileostomy |
| Toxic alcohol intoxication (methanol, ethylene glycol, diethylene glycol, propylene glycol) | Pseudoaldosteronism type I | Diabetic ketoacidosis |
| Pyroglutamic acidosis | Pseudoaldosteronism type II (Gordon’s syndrome) | Toluene intoxication |
| Fasting ketoacidosis | Drugs (spironolactone, prostaglandin inhibitors, triamterene, amiloride, trimethoprim, pentamidine, ciclosporin) | Lactic acidosis |
| Toluene intoxication |
Adverse effects
| Acute metabolic acidosis | Chronic metabolic acidosis |
|---|---|
| Impaired leukocyte function | Generation or exacerbation of bone disease |
| Predisposition to ventricular arrhythmias | Growth retardation (in children) |
| Arterial vasodilation and hypotension | Impaired glucose tolerance |
| Resistance to action of infused catecholamines | Acceleration of progression of kidney disease |
| Resistance to action of insulin | Increased muscle wasting |
| Suppression of lymphocyte function | Reduced albumin synthesis |
| Impaired cellular energy production | Enhanced production of β2-microglobulin |
| Stimulation of apoptosis | |
| Changes in mental status | |
| Stimulation of interleukin production | |
| Alteration in oxygen binding to hemoglobin | |
| Venoconstriction | |
| Decreased cardiac contractility and cardiac output |
Diagnosis
- History: Identify potential causes (vomiting, diarrhea, medications, possible overdoses, chronic conditions such as diabetes mellitus)
- Physical examination: dry mucus membranes in diabetic ketoacidosis, compensatory hyperventilation
- Lab tests;
- Blood pH <7.35
- pCO2:
- >40-45: respiratory acidosis
- <40: metabolic acidosis
- Anion gap
- Anion gap = Na+ – (Cl- + HCO3-)
- Normal anion gap = 12
- Anion gap >12: Anion gap metabolic acidosis
- Respiratory compensation
- Winter’s formula: Expected CO2 = (HCO3- x 1.5) + 8 +/- 2
- If pCO2 is within the predicted range, there is no additional respiratory disturbance
- If pCO2 is greater than expected, there is an additional respiratory acidosis
- If pCO2 is less than expected, there is an additional respiratory alkalosis
- Additional metabolic disturbances
- If anion gap is present, determine delta gap
- Delta gap = Delta anion gap – Delta HCO3- = (anion gap – 12) – (24 – HCO3-)
- Delta gap < -6: Non anion gap metabolic acidosis
- Delta gap >6: underlying metabolic alkalosis
- Delta gap between -6 and 6: only anion gap metabolic acidosis
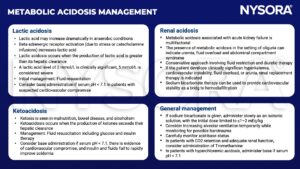
Management
- Address the cause of acidosis
- Fluid resuscitation and electrolyte imbalance correction for sepsis and diabetic ketoacidosis
- Antidotes for poisoning, dialysis, antibiotics, bicarbonate administration
Suggested reading
- Burger MK, Schaller DJ. Metabolic Acidosis. [Updated 2022 Jul 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482146/
- Fleisher, Lee A., and Stanley H. Rosenbaum. Complications in Anesthesia. Elsevier, 2018.
- Kraut, J., Madias, N. Metabolic acidosis: pathophysiology, diagnosis and management. Nat Rev Nephrol 6, 274–285 (2010).
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







