Explore NYSORA knowledge base for free:

Master your emergency diagnostics skills on the go!

Convenience meets excellence with immersive walkthroughs to the most commonly used POCUS techniques, accompanied by proprietary NYSORA learning aids and clinical pearls.


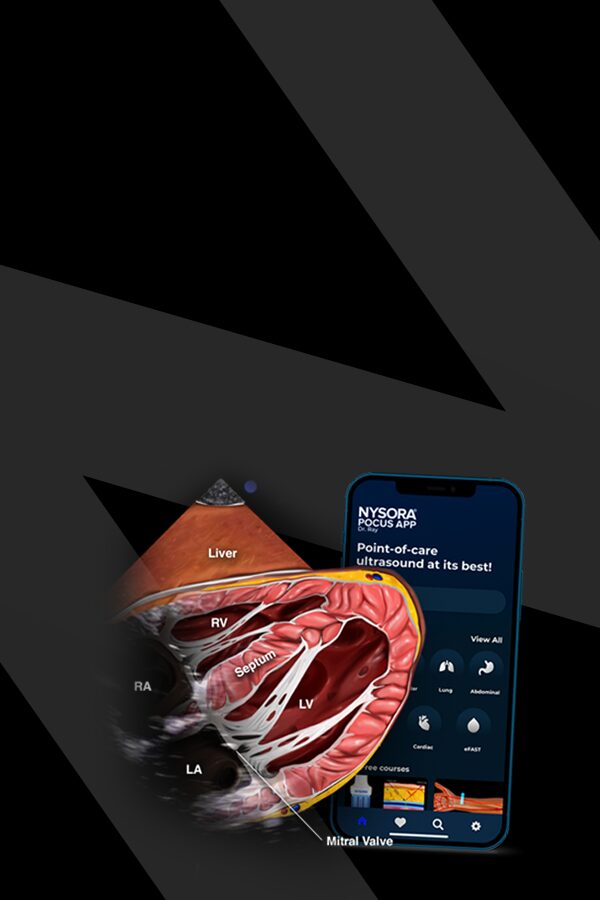
We recently partnered with Dr. Ray on POCUS. He is an anesthesiologist and critical care physician and he explains that the transition from regional anesthesia into POCUS is a natural step that considerably changes your practice. Therefore, we designed an app together to empower healthcare professionals with advanced guidance on POCUS wherever they go. We sat down with him to discuss POCUS, its history, and NYSORA’s role in the app publication.
The NYSORA POCUS (Point-of-Care Ultrasound) App is a mobile-friendly, expert-designed resource for healthcare professionals performing bedside ultrasound. It offers step-by-step protocols, high-quality ultrasound images, instructional animations, and clinical tips to optimize diagnostic accuracy and procedural confidence in emergency, critical care, and perioperative settings.
The app is ideal for anesthesiologists, emergency physicians, intensivists, internists, medical residents, and any healthcare professional utilizing POCUS for diagnosis and procedural guidance.
The objective of point-of-care ultrasound (POCUS) is to facilitate rapid clinical decision-making by providing real-time diagnostic information directly at the patient’s bedside. It allows healthcare providers to quickly assess patients, guide interventions, monitor treatment responses, and expedite patient care, particularly in critical or emergency situations.
The app includes:
The NYSORA POCUS App provides quick access to expertly-curated content, helping you:
Absolutely. The app is designed as a real-time reference tool, offering concise and structured guidance that can be used directly at the bedside.
NYSORA regularly updates the app to reflect the latest research, best practices, and clinical guidelines. Subscribed users receive these updates automatically, ensuring access to the latest updates and techniques.
Download the NYSORA POCUS App from your preferred app store, create an account, and explore the free content. For extended features, subscribe to unlock the full library and advanced tools.
Yes. The app includes high-quality instructional videos and animations demonstrating scanning techniques.
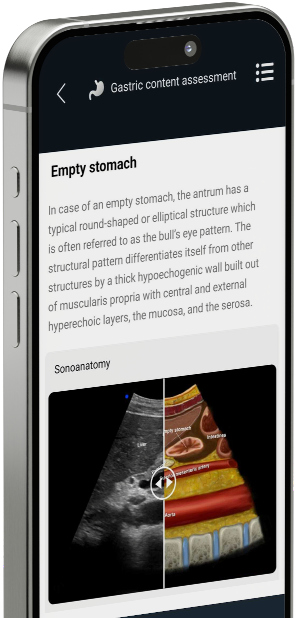
Yes. The app features detailed anatomical illustrations and NYSORA’s unique “reverse ultrasound anatomy” illustrations, helping you quickly recall sonographic patterns.
These are proprietary, revolutionary NYSORA educational tools. They take you from the ultrasound image to an illustrated anatomy view—and back again. This approach reinforces crucial anatomical knowledge and helps you recognize sonoanatomy patterns.
The app is designed to be highly practical, offering direct clinical applications and hands-on guidance for bedside ultrasound assessment and interventions.
Yes. The app includes interactive tools such as animations, videos, and self-assessment quizzes, making it easier to gain a thorough understanding and retain knowledge.
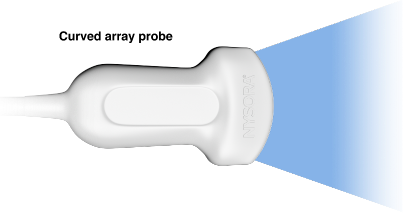
The app covers:
The app can be used in multiple ways:
1.Pre-scan review – Quickly review scanning protocols before performing an exam.
2.Live guidance – Follow step-by-step instructions while scanning.
3.Skill development – Improve diagnostic accuracy with expert insights and pathology recognition tools.
It’s a mobile-friendly reference tool offering:
The NYSORA POCUS App is developed by NYSORA’s team of experts. The content is rigorously reviewed and updated to provide evidence-based, clinically relevant information trusted by healthcare professionals worldwide.