Learning objectives
- Discuss the potential for obstetric complications after trauma
- Outline the complex management challenges of trauma during pregnancy
Definition and mechanisms
- Trauma is the leading cause of nonobstetric mortality and affects 7% of all pregnancies
- The most common traumatic injuries are motor vehicle crashes, assaults, falls, or partner violence
- Major trauma has been associated with 7 percent of maternal and 80 percent of fetal mortality
- Placental abruption is the most common cause of fetal death:
- First trimester: the thick-walled uterus is protected from trauma by the pelvic girdle
- Second trimester: the fetus is protected by relatively abundant amniotic fluid volume
- Third trimester: the thin-walled uterus is exposed to blunt and penetrating abdominal trauma
- Pregnant trauma patients should be approached and managed like any other trauma patient using a standard ABCD approach
- Clinical decision-making is complicated by:
- The needs of both mother and fetus must be considered
- Anatomical and physiological changes in pregnancy can mask or mimic injury
- Life-threatening obstetric complications can occur even after seemingly minor trauma and may require urgent delivery of the fetus
- Fetal injury can predominate of that the mother
- Establishing maternal stability may not be possible without obstetric intervention
Complications
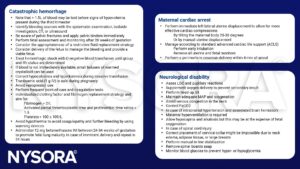
- Fetomaternal hemorrhage
- Placental abruption
- Uterine rupture
- Preterm labor
- Spontaneous miscarriage
- Pelvic fracture
Injury severity score
- The same injury severity score applies to pregnant women as nonpregnant women
Physiological changes of pregnancy
| System | Changes | Implications |
|---|---|---|
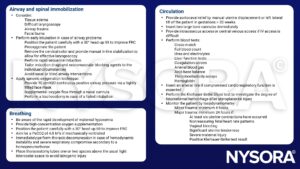
| Pulmonary system | ↑ Tidal volume The respiratory rate is unchanged ↓ FRC ↑ Oxygen consumption ↑ Minute ventilation ↓ Arterial CO2 tension ↓ Thoracic compliance Elevated diaphragm | Apply supplementary oxygen to avoid hypoxia Consider desaturation Bag mask ventilation may be difficult Place chest drains higher (3rd or 4th intercostal space) |
| Airway | ↑ Airway edema ↑ Vascular engorgement ↑ Tissue friability ↑ Breast size and neck adiposity ↑ Aspiration risk | Difficult intubation Consider cricoid pressure insert early NGT |
| Cardiovascular system | ↑ Plasma volume (40-50%) ↑ Heart rate (15-25%) ↑ Cardiac output (50%) ↓ SVR (20%) | Increased blood volume may initially mask the shock Supine hypotension due to IVC compression may reduce CO |
| Hematological changes | Hypercoagulability Anemia Thrombocytopenia ↑ Factors VII, VIII, IX, X, XII, von Willebrand, and fibrinogen ↓ aPTT, PT, and INR | All Rhesus-negative mothers should receive anti-D within 72 hours of injury Consider rhesus status when initiating blood product transfusion |
| Renal system | ↑ Renal blood flow ↑ Glomerular filtration rate (60%) ↓ Serum creatinine and bicarbonate | |
| Gastrointestinal system | ↓ Esophageal sphincter tone Cephalad displacement of the stomach ↑ Intra-gastric pressure Delayed gastric emptying | Perform early gastric decompression with NGT The bladder becomes an intra-abdominal organ after 1st trimester Other abdominal organs are displaced by the uterus |
See also physiological changes during pregnancy
Management
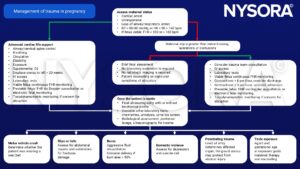
Discharge criteria:
- Resolution of contractions
- A reassuring fetal heart tracing
- Intact membranes
- No vaginal bleeding
- No uterine tenderness
- Administer Rh immune globulin therapy to all Rh-negative patients unless the injury is remote from the uterus
Anesthetic management
Suggested reading
- Irving, T., Menon, R., Ciantar, E., 2021. Trauma during pregnancy. BJA Education 21, 10–19.
- Huls CK, Detlefs C. Trauma in pregnancy. Semin Perinatol. 2018;42(1):13-20.
- Jain V, Chari R, Maslovitz S, et al. Guidelines for the Management of a Pregnant Trauma Patient. J Obstet Gynaecol Can. 2015;37(6):553-574.
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com