Learning objectives
- Describe the definition and risk factors of perioperative stroke
- Diagnose perioperative stroke
- Manage perioperative stroke
Background
- Perioperative stroke is a devastating complication of surgery
- Defined as an ischemic or hemorrhagic brain infarction that occurs during surgery or within 30 days of surgery
- Overt stroke: Acute brain infarct with clinical manifestation lasting longer than 24 hours
- Covert stroke: Infarct that is not recognized at the time of onset
- Incidence 0.1-1.9%
- Higher morbidity and mortality rates compared to stroke unrelated to surgery
Risk factors
| Patient factors | Surgical factors |
|---|---|
| Increasing age | Thoracic surgery |
| History of prior stroke or TIA | Transplant surgery |
| Hypertension | Endocrine surgery |
| History of atrial fibrillation | Burn surgery |
| Valvular disease | Otolaryngology surgery |
| Cardiovascular disease | Hemicolectomy |
| Renal disease | |
| Diabetes mellitus | |
| Smoker or COPD | |
| Patent foramen ovale | |
| Migraine with or without aura |
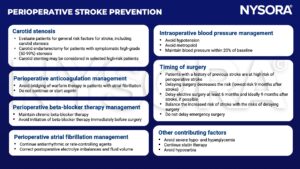
Prevention
Postoperative evaluation
- The modified National Institutes of Health Stroke Scale (NIHSS) can be used to assess patients with suspected perioperative stroke
- 0 = no stroke
- 1–4 = minor stroke
- 5–15 = moderate stroke
- 15–20 = moderate/severe stroke
- 21–42 = severe stroke
Item Score
Level of consciousness questions 0 = Answers both correctly
1 = Answers one correctly
2 = Answers neither correctly
Level of consciousness commands 0 = performs both tasks correctly
1 = performs one task correctly
2 = perform neither task
Gaze 0 = Normal
1 = Partial gaze palsy
2 = Total gaze palsy
Visual fields 0 = No visual loss
1 = Partial hemianopsia
2 = Bilateral hemianopsia
Left arm 0 = No drift
1 = Drift before 10 s
2 = Fails before 10 s
3 = No effort against gravity
4 = No movement
Right arm Same scoring as left arm
Left leg Same scoring as left arm
Right leg Same scoring as left arm
Sensory 0 = Normal
1 = Abnormal
Language 0 = Normal
1 = Mild aphasia
2 = Severe aphasia
3 = Mute
Neglect 0 = Normal
1 = Mild
3 = Severe
Management
- Early diagnosis is key (<25 min after symptom onset)
- Emergency non-contrast CT scan to discriminate between ischemic stroke from intracranial hemorrhage and nonvascular causes of neurologic symptoms (e.g., tumors)
- Multimodal CT and MRI may provide additional information
- Emergency treatment (<60 min after symptom onset):
- Move patient to acute stroke unit
- Correction of postoperative causes of hypotension (volume depletion, blood loss, myocardial ischemia, arrhythmias)
- Treat fever
- Cardiac monitoring and treatment of arrhythmias should they occur
- Intravenous thrombolysis may be beneficial
- Intraarterial thrombolysis can be administered within 6 hours of symptom onset, either alone or in conjunction with intravenous thrombolysis
- Aspirin can be used when deemed safe
- Mechanical thrombectomy in patients with large vessel occlusion, between 6 and 24 hours after symptom onset
Suggested reading
- Ng JLW, Chan MTV, Gelb Adrian W, Warner David S. Perioperative Stroke in Noncardiac, Nonneurosurgical Surgery. Anesthesiology. 2011;115(4):879-90.
- Lindberg AP, Flexman AM. Perioperative stroke after non-cardiac, non-neurological surgery. BJA Educ. 2021;21(2):59-65.
- Benesch C, Glance LG, Derdeyn CP, Fleisher LA, Holloway RG, Messé SR, et al. Perioperative Neurological Evaluation and Management to Lower the Risk of Acute Stroke in Patients Undergoing Noncardiac, Nonneurological Surgery: A Scientific Statement From the American Heart Association/American Stroke Association. Circulation. 2021;143(19):e923-e46.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







