Learning objectives
- Definition of sepsis
- Diagnostic features of sepsis
- Management of sepsis
Definition and mechanisms
- Sepsis is a dysregulated systemic response to infection that is associated with organ dysfunction
- Quick sequential organ failure assessment (qSOFA) criteria:
- Altered mental status (GCS score < 15)
- Systolic blood pressure < 100 mmHg
- Respiratory rate > 22 breaths per min
- Septic shock is defined as low blood pressure due to sepsis that does not improve after fluid replacement
- Characterized by high morbidity and mortality (30-50% of affected patients)
- Septic patients are at risk for secondary injuries
- Bacteria, fungi, and viruses can all cause sepsis
Signs and symptoms
- Fever or hypothermia
- Increased heart rate
- Increased breathing rate
- Confusion
- Hypotension
- Sweating
- Edema
- Low urine output
Risk factors
- People older than 65 years old, newborns and infants, and pregnant people
- Medical conditions such as diabetes, obesity, cancer, and kidney disease
- A weakened immune system
- People who are in the hospital for other medical reasons
- Severe injuries, such as large burns or wounds
- Patients with catheters, IVs, or breathing tubes
Diagnostic features
| Organ system | Alteration of dysfunction |
|---|---|
| Neurological | Delirium Altered mental status Ischemia Formation of blood clots in small blood vessels Microabscesses Multifocal necrotizing leukoencephalopathy |
| Cardiovascular | Vasodilation Hypovolemia Cardiac dysfunction Systolic and diastolic dysfunction |
| Pulmonary | Tachypnea Poor gas exchange Acute Respiratory Distress Syndrome |
| Gastrointestinal | Ileus Hyperbilirubinemia |
| Kidney | Oliguria Elevated plasma urea and creatinine Volume overload |
| Hepatic | Disruption of blood clotting Elevated unconjugated serum bilirubin levels |
| Hematological | Perioperative anemia Thrombocytopenia Coagulopathy Disseminated Intravascular Coagulation (DIC) |
| Endocrine and metabolic | Hyperglycemia Sick euthyroid syndrome Elevated lactate |
| Infectious disease | Leucocytosis Elevated inflammatory mediators |
Treatment
- Aggressive source control, resuscitation, and antibiotic therapy are the mainstays of management
- Be aware of subtle changes such as hyperglycemia, ileus, mental status changes, and potential sources of infections

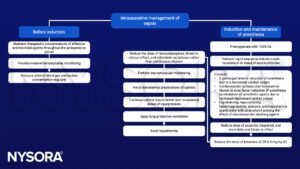
Anesthetic management

Suggested reading
- Ammar, M.A., Ammar, A.A., Wieruszewski, P.M. et al. Timing of vasoactive agents and corticosteroid initiation in septic shock. Ann. Intensive Care 12, 47 (2022).
- Charlton, M., Thompson, J.P., 2019. Pharmacokinetics in sepsis. BJA Education 19, 7–13.
- Gyawali B, Ramakrishna K, Dhamoon AS. Sepsis: The evolution in definition, pathophysiology, and management. SAGE Open Med. 2019;7:2050312119835043.
- Keeley A, Hine P, Nsutebu EThe recognition and management of sepsis and septic shock: a guide for non-intensivistsPostgraduate Medical Journal 2017;93:626-634.
- Nunnally, M.E., 2016. Sepsis for the anaesthetist. British Journal of Anaesthesia 117, 44–51.
- Eissa D, Carton EG, Buggy DJ. Anaesthetic management of patients with severe sepsis. Br J Anaesth. 2010;105(6):734-743.
We would love to hear from you. If you should detect any errors, email us [email protected]








