Learning objectives
- Recognize hypoxemia
- Differential diagnosis of hypoxemia
- Management of hypoxemia
Definition and mechanism
- A decrease in the partial pressure of oxygen in the blood
- Severe when oxygen saturation falls below 90%
- Acute hypoxemia will eventually cause circulatory arrest due to myocardial hypoxia with:
- Irreversible cardiac damage
- Loss of consciousness within 10 seconds
- Irreversible brain damage within 4-5 minutes
Signs and symptoms
- Shortness of breath
- Increased breathing rate
- Headache
- Coughing
- Tachycardia
- Use of chest and abdominal muscles to breath
- Cyanosis
- Hemoptysis
Diagnosis
- Pulse oximetry
- Arterial blood gas test
- Six-minute walk test
Differential diagnosis
| Equipment failure | |
| Hypoventilation | Low TV or RR Ventilator dyssynchrony Circuit leak Obstructed ETT |
| Ventilation-perfusion mismatch | Bronchospasm Mainstem intubation Pulmonary edema Aspiration Atelectasis Pneumothorax Pleural effusion |
| Right-to-left shunt | Intracardiac shunting |
| Diffusion impairment | Pulmonary edema Pneumonia |
| Low PO2 | Increased dead space Pulmonary embolism Reduced cardiac output |
| Increased metabolic O2 demand | Malignant hyperthermia Sepsis Neuroleptic malignant syndrome |
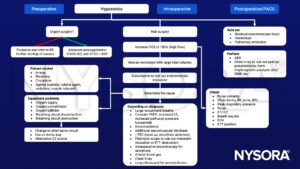
Management
Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Rozé H, Lafargue M, Ouattara A. Case scenario: Management of intraoperative hypoxemia during one-lung ventilation. Anesthesiology. 2011;114(1):167-174.
We would love to hear from you. If you should detect any errors, email us at [email protected]








