Learning objectives
- Identify and treat underlying causes of peripartum cardiac arrest
- Manage patients presenting with peripartum cardiac arrest
Background
- Peripartum cardiac arrest is a rare event with an incidence of one in 12,000 – 36,000 women per year
- A prompt, coordinated response by a multidisciplinary team is essential
- Need to consider two patients: The mother and de fetus
- The maternal cardiac arrest response team and protocols should be regularly reviewed with didactic and simulation sessions
- Strong leadership and teamwork are essential
Causes & treatments
| Cause of cardiac arrest | Treatment | |
|---|---|---|
| Complications of anesthesia | High neuraxial block | Treat hypotension aggressively (e.g., low-dose adrenaline) Support airway and breathing |
| Loss of airway, aspiration, respiratory depression | Support airway and breathing Difficult airway algorithm |
|
| Hypotension | Treat with vasopressors Lower head of bed to improve cerebral perfusion Volume replacement Obtain more intravenous access |
|
| Local anesthetic systemic toxicity (LAST) | Give intralipid Consider cardiopulmonary bypass or ECMO |
|
| Bleeding | Coagulopathy | Fibrinogen replacement Fresh frozen plasma Cryoprecipitate Platelets Consider tranexamic acid 1 g IV |
| Uterine atony | Give uterotonics Bakri balloon Compression suture Uterine artery embolisation Hysterectomy |
|
| Placenta accreta | Consider uterine artery embolisation Consider hysterectomy |
|
| Placental abruption | Delivery if indicated Monitor for coagulopathy |
|
| Placenta previa | Delivery if indicated Prepare for lower uterine segment atony |
|
| Uterine rupture | Uterine repair or hysterectomy | |
| Trauma | Call general surgeon Activate massive transfusion |
|
| Transfusion reaction | Stop transfusion Notify blood bank Adrenaline Steroids Send tryptase |
|
| Cardiovascular | Cardiomyopathy | Inotrope infusion Call for ECMO |
| Myocardial infarction | Inotrope infusion Call for ECMO Call for cardiac surgeon Call cardiac catheterization laboratory Send cardiac enzymes |
|
| Aortic dissection | Call cardiac surgeon Activate massive transfusion |
|
| Arrhythmias | Ventricular fibrillation: Defibrillate Unstable ventricular tachycardia: Amiodarone, lidocaine Torsade de pointes: Defibrillate, magnesium Stable ventricular tachycardia: Amiodarone, lidocaine Supraventricular tachycardia: Adenosine Atrial fibrillation: Amiodarone, cardioversion |
|
| Medications | Anaphylaxis | Adrenaline Steroids Diphenhydramine Ranitidine |
| Illicit | Opioid overdose: Naloxone Benzodiazepine overdose: Flumazenil Cocaine coronary vasospasm: Oxygen, aspirin, nitrates, thrombolytic therapy, or acute percutaneous coronary intervention |
|
| Drug error | Identify, discontinue agent and treat | |
| Magnesium toxicity | Stop magnesium Give calcium chloride 10 mL in 10% solution or calcium gluconate 30 mL in 10% solution |
|
| Insulin overdose | Give glucose/dextrose Glucagon |
|
| Oxytocin overdose | Treat hypotension | |
| Embolic | Pulmonary embolus | Call Interventional radiology Call cardiac surgeon Prepare catheterisation laboratory Echocardiography Start heparin IV Consider thrombolytics in cardiac arrest Nitric oxide |
| Coronary thrombus | Call cardiac surgeon Catheterisation laboratory Nitroglycerine |
|
| Amniotic fluid embolism/Anaphylactoid syndrome of pregnancy | Adrenaline Initiate cardiopulmonary resuscitation Call for extracorporeal membrane oxygenator Call for transesophageal echocardiography Prepare for coagulopathy and need for massive transfusion protocol Consider unproven ‘A-OK’ therapy: atropine, ondansetron, ketorolac Consider steroids Consider nitric oxide |
|
| Venous air embolism | Flood field if uterine venous sinuses open Internalise uterus |
|
| Fever | Infection, sepsis | Give broad spectrum antibiotics Fluids, volume replacement Vasopressors Place arterial line Perform echocardiogram Inotrope if low cardiac output |
| General non-obstetric causes of cardiac arrest | Hypotension | Treat with vasopressors Lower head of bed to improve cerebral perfusion Fluids, volume replacement Obtain more intravenous access Call for transthoracic echocardiography |
| Hypoxia | Airway control 100% oxygen |
|
| Hypothermia | Warm patient Warm fluids Blankets Increase room temperature |
|
| Hyperkalemia | Calcium Insulin and glucose Furosemide Albuterol Sodium bicarbonate to correct acidosis Intubate and hyperventilate Polystyrene sulphonate (potassium binder) Consider hemodialysis |
|
| Hypoglycemia | Give glucose/dextrose Glucagon |
|
| Hypercarbia/acidosis | Intubate trachea and optimize ventilation Determine cause of acidosis Sodium bicarbonate |
|
| Thrombus | See pulmonary embolus above | |
| Trauma | Call general or trauma surgeon | |
| Toxin | Give antidote if agent known |
|
| Tension pneumothorax | Needle decompression Insert chest tube |
|
| Tamponade | Call for ECMO Call cardiac surgeon |
|
| Hypertension | Pre-eclampsia/eclampsia/HELLP | Antihypertensive agents: labetalol (avoid in asthmatics), hydralazine, nicardipine Magnesium |
| Intracranial hemorrhage with increased intracranialpressure | Call neurosurgeon Blood pressure goal: systolic <140 mmHg Elevate head of bed 30° Reverse coagulopathy if present Hypertonic saline/mannitol |
ECMO, extracorporeal membrane oxygenation; HELLP, hemolysis, elevated liver enzymes, low
platelet count.
Management
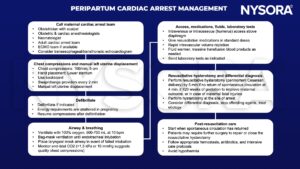
ECMO, extracorporeal membrane oxygenation.
Suggested reading
- Madden AM, Meng ML. Cardiopulmonary resuscitation in the pregnant patient. BJA Educ. 2020;20(8):252-258.
- Jeejeebhoy FM, Zelop CM, Lipman S, Carvalho B, Joglar J, Mhyre JM, et al. Cardiac Arrest in Pregnancy. Circulation. 2015;132(18):1747-73.
We would love to hear from you. If you should detect any errors, email us [email protected]








