Learning objectives
- Describe the risk factors and symptoms of peripartum cardiomyopathy
- Diagnose peripartum cardiomyopathy
- Manage patients with peripartum cardiomyopathy
Background
- Peripartum cardiomyopathy (PPCM) is a rare cause of cardiomyopathy occurring during late pregnancy or in the early postpartum period
- Characterized by significant left ventricular dysfunction and heart failure in the peripartum period in the absence of other identifiable causes of heart failure
- Potentially life-threatening condition
- Left ventricle ejection fraction is nearly always less than 45%
- Etiology is unclear but likely multifactorial (hormonal, inflammatory, genetic,…)
Risk factors
- African descent
- Increasing age
- Pregnancy-related hypertension
- Multiparity
- Multiple gestations
- Obesity
- Chronic hypertension
- Chronic tocolytics use
- Cocaine use
Signs & Symptoms
- Paroxysmal nocturnal dyspnea
- Pedal edema
- Orthopnea
- Dyspnea on exertion
- Dry cough
- Palpitations
- Increase in abdominal girth
- Lightheadedness
- Chest pain
- Jugular venous distentions
- Displaced apical impulse
- Third heart sound
- Mitral regurgitation murmurs
Diagnosis
- Diagnosis is based on exclusion
- Differential diagnoses:
- Pulmonary embolism
- Severe sepsis
- Amniotic fluid embolism
- Preeclampsia/pregnancy-induced hypertensive disease
- Arrhythmias
- Severe anemia
- Myocardial infarction
- Dilated cardiomyopathy of other etiologies
- Diagnostic tests:
- Routine blood tests
- Evaluate for anemia, electrolyte abnormalities, endocrine conditions, renal or liver dysfunction
- Brain natriuretic peptide (BNP) is commonly elevated in patients with heart failure and PPCM
- Chest radiography
- Cardiomegaly and/or pulmonary edema are suggestive of heart failure but nonspecific to PPCM
- ECG
- Sinus tachycardia, supraventricular tachycardia, ventricular tachycardia, ST segment and T wave abnormalities, dilation of chambers, and QRS prolongation may be observed but are nonspecific
- Echocardiography
- Left ventricular ejection fraction <45%: Requirement for PPCM diagnosis
- Evaluation of other etiologies such as valvular diseases or structural abnormalities
- Ventricle/atrium dilation and left ventricular thrombus or atrial thrombosis may be present
- Cardiac MRI
- Evaluation of other causes of heart failure
- Cardiac catheterization
- Only for selected patients
- Left heart catheterization is indicated in patients with suspected ischemic cardiomyopathy
- Routine blood tests
Management
Management is similar to that of other causes of heart failure
- Pharmacological
- Angiotensin-converting enzyme (ACE) inhibitors: First-line treatment postpartum, contraindicated during pregnancy
- Hydrazaline and nitrate therapy can be used safely during pregnancy
- Beta-blockers
- Digoxin (carefully monitor plasma levels)
- Loop diuretics (e.g., furosemide)
- Avoid calcium channel blockers and aldosterone antagonists
- Thromboprophylactic low molecular weight heparin
- Non-pharmacological:
- Non-invasive ventilation or intubation
- Inotropic support
- Intra-aortic balloon pump, left ventricular assist device or extracorporeal membrane oxygenation may be required in severe cases
- Heart transplantation in severe cases who do not respond to therapy
- Implantable defibrillator or cardiac resynchronization in patients with chronic functional impairment
Prognosis
| Good prosnosis | Small left ventricular diastolic dimension (less than 5.5cm) |
| Left ventricular ejection fraction greater than 30% to 35% and fractioning of shortening greater than 20% at the time of diagnosis | |
| Absence of troponin elevation | |
| Absence of left ventricular thrombus | |
| Non-African ethnicity | |
| Poor prognosis | QRS greater than 120 ms |
| Delayed diagnosis | |
| High New York Heart Association (NYHA) class | |
| Multiparity | |
| African descent |
Complications
- Thromboembolism
- Arrhythmias
- Progressive heart failure
- Misdiagnosis as preeclampsia
- Fetal distress from hypoxia
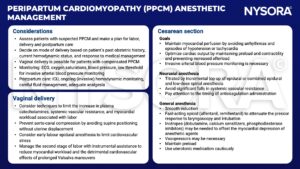
Anesthetic management
Suggested reading
- Rodriguez Ziccardi M, Siddique MS. Peripartum Cardiomyopathy. [Updated 2022 Jul 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482185/
- Honigberg MC, Givertz MM. Peripartum cardiomyopathy. BMJ. 2019;364:k5287. Published 2019 Jan 30. doi:10.1136/bmj.k5287
- Thompson L, Hartsilver E. Peripartum cardiomyopathy. WFSA. https://resources.wfsahq.org/atotw/peripartum-cardiomyopathy/#:~:text=Titrated%20neuraxial%20anaesthesia%2C%20by%20incremental,agents%20that%20reduce%20myocardial%20contractility. Published February 24, 2015. Accessed February 13, 2023.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com