Learning objectives
- Understand the common causes of postpartum hemorrhage (PPH)
- Management of PPH
Definition and mechanisms
- Abnormal blood loss within 24 hours after birth
- Vaginal delivery: estimated blood loss (EBL) > 500 ml
- Post-C-section: EBL > 1000 ml
- PPH is the leading cause of maternal mortality in low-income countries and the primary cause of nearly one-quarter of all maternal deaths globally
Signs and symptoms
- EBL > 500
- Tachycardia
- Hypotension
- Delayed capillary refill
- Decreased urine output
- Pallor
- Lightheadedness
- Palpitations
- Confusion
- Syncope
- Fatigue
- Air hunger
- Diaphoresis
Risk factors
| Medical or surgical history | Previous postpartum hemorrhage Leiomyomata Previous Caesarean delivery or other uterine instrumentation |
| Fetal issues | Multifetal gestation Polyhydramnios Large-for-gestational-age fetus Fetal macrosomia |
| Maternal issues | Hypertensive disorders of pregnancy Perioperative anemia Inherited coagulopathy such as Von Willebrand’s Disease (VWD) Acquired coagulopathy such as HELLP syndrome Trial of labor after Caesarean delivery Prolonged labor Induction and augmentation of labor The arrest of progress during the second stage of labor The prolonged third stage of labor Instrumentation during delivery |
| Placental/uterine issues | Placental abruption Placenta praevia Retained placenta Chorioamnionitis Acute Uterine inversion Subinvolution of the uterus |
However, 20% of postpartum hemorrhage occurs in women with no risk factors
Causes
The four T’s mnemonic of postpartum hemorrhage:
| Tonus | Atonic uterus | 70% |
| Tissue | Retained placenta, invasive placenta | 10% |
| Trauma | Laceration, hematoma, Uterine inversion, rupture | 20% |
| Thrombi | Coagulopathy | 1% |
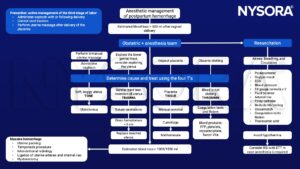
Anesthetic management
Suggested reading
- Watkins EJ, Stem K. Postpartum hemorrhage. JAAPA. 2020;33(4):29-33.
- Evensen A, Anderson JM, Fontaine P. Postpartum hemorrhage: prevention and treatment. Am Fam Physician. 2017; 95(7): 442-449.
- 2017. Prevention and Management of Postpartum Haemorrhage. BJOG: An International Journal of Obstetrics & Gynaecology 124, e106–e149.
- E. Mavrides, S. Allard, E. Chandraharan, P. Collins, L. Green, BJ. Hunt, S. Riris. AJ. Thomason on behalf of the Royal college of obstetricians and gynaecologists. Prevention and management of postpartum haemorrhage. BJOG 2016; 124:e 106-e149
- Anderson JM, Etches D. Prevention and management of postpartum hemorrhage. Am Fam Physician. 2007;75(6):875-882.
- WHO recommendations for the prevention and treatment of postpartum haemorrhage.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







