Learning objectives
- Describe necrotizing enterocolitis
- Recognize signs and symptoms of necrotizing enterocolitis
- Anesthetic management of an infant with necrotizing enterocolitis
Definition and mechanisms
- Necrotizing enterocolitis (NEC) is a life-threatening intestinal disease that affects premature or very low birth-weight infants
- It is the most common gastrointestinal (GI) emergency in NICUs → leading cause of long-term disability in preterm infants
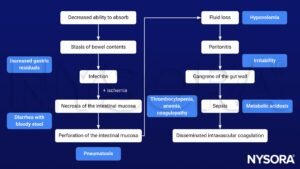
- Inflammation of the intestine leads to bacterial invasion causing cellular damage and cellular death, and necrosis of the colon and intestine → as NEC progresses, it may lead to intestinal perforation, causing peritonitis, sepsis, and death
- Mortality up to 30%
Signs and symptoms
- Abdominal pain and distention
- Changes in heart rate, blood pressure, and breathing
- Diarrhea with bloody stool
- Increased gastric residuals
- Vomiting of bile
- Lethargy
- Feeding intolerance
- Failure to thrive
- Hyperglycemia
- Temperature instability
- In severe cases: Hypotension, disseminated intravascular coagulation, and metabolic acidosis
Diagnosis
Bell’s stages of NEC
- Stage I (suspected disease): Mild systemic signs (apnea, bradycardia, temperature instability, lethargy), mild GI signs (abdominal distension, increased gastric residuals, bloody stools), non-specific or normal radiologic signs
- Stage II (definite disease): Mild systemic signs with additional GI signs (absent bowel sounds, abdominal tenderness), specific radiological signs (dilated loops of intestines, pneumatosis intestinalis or portal venous air), abnormal laboratory investigations (e.g., metabolic acidosis, thrombocytopenia)
- Stage III (advanced disease): Severe systemic illness (with hemodynamic instability), additional GI signs (gross abdominal distension, peritonitis), severe radiological signs (pneumoperitoneum), additional laboratory findings (e.g., metabolic and respiratory acidosis, disseminated intravascular coagulation)
Complications
- Abdominal infection: Peritonitis increases the risk of sepsis
- Intestinal strictures: A stricture narrows the intestines
- Short bowel (short-gut) syndrome: Results in malabsorption
- Growth failure, poor neurodevelopmental outcomes, and developmental delay: Mainly in infants requiring surgery
Risk factors
- Prematurity
- Low birth weight
- Birth asphyxia
- Hypoxemia
- Enteral feedings
- Cyanotic heart disease
- Patent ductus arteriosus
- Exchange transfusion
- Prolonged rupture of membranes
Pathophysiology
Treatment
- Medical management will avoid surgery in 85% of cases
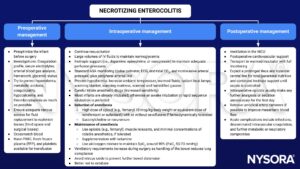
- Fluid resuscitation
- Stop enteral nutrition
- Decompress the stomach with a nasogastric tube
- Antibiotics
- Packed red blood cells (PRBC) and platelet transfusions
- Surgery
- Exploratory laparotomy removal of the gangrenous bowel
- Ileostomy
- Peritoneal drain
- Indications for surgery
Anesthetic considerations
- Premature infant considerations
- Increased risk of aspiration: Bowel obstruction, dilated bowel loops, pneumatosis intestinalis
- Associated multisystem derangements: Hypoxia, sepsis, hypovolemia, disseminated intravascular coagulation, thrombocytopenia, metabolic acidosis
- Associated conditions: Birth asphyxia, hypotension, respiratory distress syndrome, patent ductus arteriosus, recurrent apnea, intestinal ischemia, systemic infections
Management
Prognosis
Long-term survival depends on
- Degree of prematurity
- Associated congenital anomalies
- Degree of surviving bowel
- Total length of affected bowel
Prevention
- Breast milk
- Probiotics
Suggested reading
- Houck PJ. Chapter 175. Necrotizing Enterocolitis. In: Atchabahian A, Gupta R. eds. The Anesthesia Guide. McGraw Hill; 2013. Accessed February 13, 2023. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=572§ionid=42543766
- Sodhi P, Fiset P. Necrotizing enterocolitis. Continuing Education in Anaesthesia Critical Care & Pain. 2012;12(1):1-4.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com