Learning objectives
- Describe ankylosing spondylitis
- Recognize the symptoms and signs of ankylosing spondylitis
- Anesthetic management of a patient with ankylosing spondylitis
Definition and mechanisms
- Ankylosing spondylitis (AS), autoimmune seronegative spondyloarthropathy, is a painful chronic inflammatory arthritis characterized by exacerbations (flares) and quiescent periods
- AS primarily affects the spine and sacroiliac joints, eventually causing fusion and rigidity of the spine → bamboo spine
- Joint mobility in the affected areas worsens over time
- The areas most commonly affected are
- Sacroiliac joints
- Vertebrae in the lower back
- Places where tendons and ligaments attach to bones, mainly in the spine
- Cartilage between the breastbone and the ribs (sternum)
- Hip and shoulder joints
- Linked to HLA-B27 gene
Signs and symptoms
Symptoms might worsen (flares), improve, or stop at irregular intervals
- Chronic dull pain in the lower back or gluteal region combined with stiffness of the lower back, especially in the morning and after periods of inactivity
- Hip pain
- Joint pain
- Neck pain
- Fatigue
- Difficulty breathing
- Loss of appetite and unexplained weight loss
- Abdominal pain and diarrhea
- Skin rash
- Vision problems
Complications
- Spinal compression fractures
- Atlanto-axial subluxation possible (21% of AS patients)
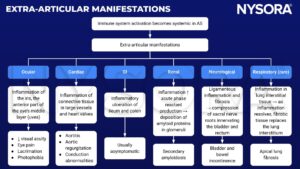
- Eye inflammation (iritis or uveitis) and sensitivity to light (photophobia)
- Fused vertebrae (ankylosis)
- Kyphosis (forward curvature of the spine)
- Osteoporosis
- Cardiovascular abnormalities: Aortic insufficiency/aortitis, arrhythmias, angina, cardiomyopathy
- Respiratory abnormalities: Chest pain that affects breathing, restrictive disease, upper lobe fibrosis
- Jaw inflammation
- Cauda equina syndrome (rare)
- Patients with AS may also have psoriasis and/or inflammatory bowel disease
Extra-articular manifestations
Treatment
- Medications: Relieve pain and reduce inflammation
- Non-steroidal anti-inflammatory drugs (NSAIDs): Ibuprofen and naproxen
- Corticosteroids: i.v. methylprednisolone
- Disease-modifying anti-rheumatic drugs (DMARDs): Sulfasalazine
- TNF-α inhibitors: Infliximab, adalimumab, and etanercept
- Exercise: To reduce pain and stiffness
- Physical therapy: Improve comfort and spinal flexibility
- Surgery (rare): Repair significantly damaged joints or correct severe bends in the spine
Management

Obstetrical anesthesia
- Complicated due to difficult airway and difficult neuraxial techniques → have multiple plans in place
- Consider paramedian approach and ultrasound guidance for neuraxial anesthesia
Keep in mind
- AS is a challenge for the anesthesiologist because the rigid, immobile, fragile spine makes intubation, general anesthesia, and neuraxial anesthesia difficult
- Awake fiberoptic intubation is the safest method of securing the airway in AS patients, but supraglottic airway devices such as laryngeal masks can also be used
- The use of alternative approaches, such as the paramedian approach or the use of ultrasound guidance, may improve success with neuraxial anesthesia in AS patients
Suggested reading
- Pahwa D, Chhabra A, Arora MK. Anaesthetic management of patients with ankylosing spondylitis. Trends in Anaesthesia and Critical Care. 2013;3(1):19-24.
- Woodward LJ, Kam PC. Ankylosing spondylitis: recent developments and anaesthetic implications. Anaesthesia. 2009;64(5):540-548.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com