Learning objectives
- Define prematurity and describe its classification
- Describe the specific anatomical, physiological, and pharmacological difficulties in premature infants
- Understand how these difficulties impact anesthesia in premature infants
Background
- Prematurity is defined as a live birth before 37 weeks of gestational age
- Moderate to late preterm: 32-37 weeks
- Very preterm: 28-32 weeks
- Extremely preterm: <28 weeks
- Preterm infants can also be categorized based on their birth weight
- Low birth weight: <2500 g
- Very low birth weight: <1500 g
- Extremely low birth weight: <1000 g
- Approximately 10% of infants are born prematurely
- The earlier the baby is born, the higher the risk of complications
- Important growth occurs in the final months and weeks of pregnancy (e.g., the brain, lungs, and liver need the final weeks of pregnancy to develop fully)
Known risk factors of premature delivery
- Previous premature birth
- Pregnancy with twins, triplets, or other multiples
- Interval of <6 months between pregnancies
- Conceiving through in vitro fertilization
- Problems with the uterus, cervix, or placenta
- Smoking and drug use
- Infections (e.g., of the amniotic fluid and lower genital tract)
- Chronic conditions (e.g., hypertension and diabetes)
- Being underweight or overweight before pregnancy
- Stressful life events
- Multiple miscarriages or abortions
- Physical injury or trauma
- Many women who have a premature birth have no known risk factors
Anatomical and physiological considerations
- Altered airway anatomy
- Respiratory derangements
- Development of conducting airways, alveoli, and pulmonary vasculature is interrupted
- Surfactant is produced in insufficient quantities until 35 weeks
- Respiratory distress syndrome
- Bronchopulmonary dysplasia
- Rapid desaturation
- Postoperative apnea
- Persistent pulmonary hypertension
- Cardiovascular derangements
- Heart rate/preload-dependent cardiac output
- Transitional circulation/patent ductus arteriosus (PDA)
- Bradycardia
- Congenital heart disease
- CNS derangements
- Intraventricular hemorrhage
- Seizures
- Cerebral palsy
- Retinopathy of prematurity
- Apnea
- Gastrointestinal derangements
- Metabolic derangements
- Impaired temperature and glucose regulation
- Prone to hypothermia
- Hyperglycemia is caused by incomplete suppression of hepatic glucose production and defective insulin secretion
- Hypoglycemia results from minimal glycogen reserves and limited ketogenesis and lipolysis
- Impaired temperature and glucose regulation
- Hematologic derangements
- Anemia
- Thrombocytopenia
- Coagulopathy
Pharmacological considerations
- Altered pharmacology
- Increased volume of distribution
- Opioid sensitivity
- Decreased clearance, protein binding, metabolism, and minimum alveolar concentration
- Drugs will accumulate with repeat doses or infusions
- Immature renal and hepatic function
Treatment
- Admission to NICU
- Supportive care
- Incubator: To maintain normothermia
- Monitoring vital signs: Blood pressure, heart rate, breathing, and temperature
- Ventilator may be used to help with breathing
- Placement of a nasogastric tube
- Fluid therapy
- Bilirubin lights: To treat infant jaundice
- Blood transfusion if needed
- Medications: To promote maturing and stimulation of normal functioning of the lungs, heart, and circulation
- Surfactant to treat respiratory distress syndrome
- Aerosolized or IV medication to strengthen breathing and heart rate
- Antibiotics to treat infections
- Diuretics to increase urine output and manage excess fluid
- Medicine to close PDA
- Surgery (e.g., PDA closure)
Management
Preoperative management
- Manage premature infants in specialized pediatric centers
- Risk stratification
- 5 times higher in-hospital mortality for non-cardiac surgery than term neonates
- Discuss proposed interventions with the surgical and NICU multidisciplinary teams and family
- Some surgical procedures can be performed in the NICU (e.g., PDA closure), especially if the patient is unstable or difficult to transport
- Preoperatively optimize respiratory, cardiovascular, hepatic, renal, and hematological derangements
- Preoperatively optimize fluid, electrolyte, and glucose derangements
- Airway and ventilation
- Assess the presence of subglottic stenosis, tracheal or laryngomalacia, frequency and severity of apneas, history of difficult intubation or ventilation
- Methylxanthine drugs to prevent apneas and facilitate extubation
- Cardiovascular system
- Inotropic support
- Echocardiography to assess ventricular function and the presence of shunts or other congenital defects
- Neurological system
- Morphine (10-40 mcg/kg/h) to sedate patients to tolerate tracheal tube
- Neurological assessment in case of preexisting neurological concerns
- Difficult IV access
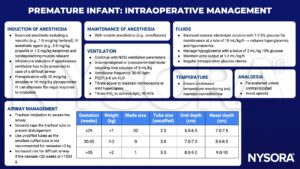
Intraoperative management
Postoperative management
- The majority of premature infants remain intubated after surgery
- Awake extubation after full reversal of neuromuscular block and adequate ventilation
- Postoperative apnea monitoring for 24-48 hours after surgery (unless if the infant is >50-60 weeks postmenstrual age and has no other risk factors for apnea)
Keep in mind
- Premature infants are a high-risk group and present with unique anatomical, physiological, and pharmacological challenges
- Anesthetic considerations are based on the physiological immaturity of various body systems, associated congenital disorders, and poor tolerance of anesthetic drugs
- The benefits of adequate anesthesia and analgesia must outweigh the risk of cardiorespiratory depression
- The main goal of anesthesia in this pediatric patient population is to titrate anesthetics to the desired effect while carefully monitoring the cardiorespiratory status
Suggested reading
- Macrae J, Ng E, Whyte H. Anaesthesia for premature infants. BJa Education. 2021;21(9):355-363.
- Taneja B, Srivastava V, Saxena KN. Physiological and anaesthetic considerations for the preterm neonate undergoing surgery. J Neonatal Surg. 2012;1(1):14.
We would love to hear from you. If you should detect any errors, email us [email protected]