Learning objectives
- Indications for a caesarean delivery
- Benefits of regional versus general anesthesia
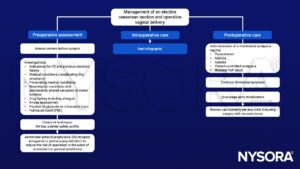
- Management of an elective caesarean section and operative vaginal delivery
- Management of an emergency caesarean section and operative vaginal delivery
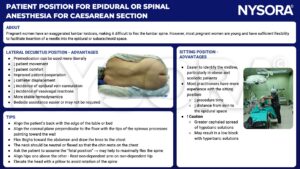
- Patient position for epidural or spinal anesthesia for caesarean delivery
Definition and mechanisms
- A surgical procedure by which one or more babies are delivered through an incision in the mother’s abdomen, often performed because vaginal delivery would put the baby or mother at risk
- Elective caesarean is the most common obstetric operation
- Planning for a caesarean section might be necessary if there are certain pregnancy complications
- Often performed as an urgent or emergency procedure
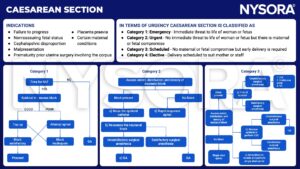
Indications
- Breech
- Multiples
- Previous caesarean section
- Maternal high blood presure
- Malplacentation (minor or major placenta praevia) and morbidly adherent placenta (placenta accreta or perccreta)
- Prevention of transmission of HIV from mother to baby
- Maternal choice
Anesthesia for caesarean section
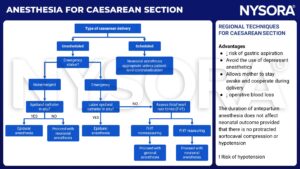
Benefits of regional versus general anesthesia
| Regional anesthesia | General anesthesia |
|---|---|
| Reduced blood loss Improved pain relief postoperatively Avoids the risk of failed intubation The mother is awake when her baby is delivered Facilitates the presence of birth partners at delivery Supports skin-to-skin contact in the operating OR | Provides anesthesia when regional techniques are contraindicated, such as when the woman has: - Abnormalities of clotting or recent thromboprophylaxis - Significant cranial or spinal abnormalities (e.g. spina bifida, chiari malformation) Alleviates profound anxiety of being awake during surgery Facilitates the management of complex cases from the outset of the procedure Eliminates any intraoperative sensation of tugging/stretching |
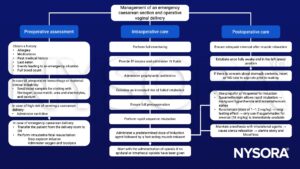
Management of an elective caesarean section and operative vaginal delivery

Management of an emergency caesarean section and operative vaginal delivery
- Four groups according to the urgency of caesarean delivery
| Category | Risk to mother and/ or baby | Indication | Target time for decision to delivery interval (DDI) |
|---|---|---|---|
| 1. Emergency | An immediate threat to life | An immediate threat to the life of the woman or fetus (e.g. severe foetal bradycardia, cord prolapse, uterine rupture, foetal blood sample pH ≤7.2) | ≤30 minutes |
| 2. Urgent | Maternal or fetal compromise | No immediate threat to life of woman or baby (e.g. APH, failure to progress) | ≤75 minutes |
| 3. Scheduled | Time for procedure to be scheduled | Requires early delivery (e.g. intrauterine growth retardation, failed induction of labor) | In the interests of mother and baby |
| 4. Elective (Management see above) | No maternal or fetal compromise | At a time to suit the woman and maternity services (breech, previous CD) | Usually after 39 weeks of gestation if possible |
Epidural top-up
- Can be used to provide anesthesia if there is a well-functioning epidural
- Can be administered in the delivery room if the anesthesiologist remains present at all times and vasopressors are immediately available
- Perform a block from sacral regions to T4 with 2 mL of LA
- Administration of the dose in 5–10 mL aliquots will help prevent hypotension or high block
- Add opioids (fentanyl 100 mcg or diamorphine 2.5-5 mg) will improve analgesia quality
Indications for general anesthesia in caesarean delivery
- If RA is contraindicated
- If mothers decline RA
- Life-threatening conditions for the mother and/or baby
- Prolonged fetal bradycardia
- Umbilical cord prolapse
- Major placental abruption (with maternal/fetal compromise)
- Uterine rupture
- Uncontrolled massive hemorrhage
Patient position for epidural or spinal anesthesia for caesarean delivery

Suggested reading
- Neall G, Bampoe S, Sultan P. 2022. Analgesia for Caesarean section. BJA Education. 22;5:197-203.
- Delgado C, Ring L, Mushambi MC. 2020. General anesthesia in obstetrics. BJA Education. 20;6:201-207.
- Adshead, D., Wrench, I., Woolnough, M., 2020. Enhanced recovery for elective Caesarean section. BJA Education 20, 354–357.
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- McGlennan A, Mustafa A. 2009. General anaesthesia for Caesarean section. Continuing Education in Anaesthesa Critical Care & Pain. 9;5:148-151.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com