Learning objectives
- Describe the causes of perioperative bleeding
- Optimize patients at risk of perioperative bleeding
- Manage perioperative bleeding
Background
- Perioperative bleeding is a complex surgical complication with a range of causes
- Usually characterized by a site of bleeding and confined exclusively to the operative site
- Can evolve into pathologic thrombosis
Causes
- Blood loss
- Hemodilution
- Acquired platelet dysfunction
- Coagulation factor consumption in extracorporeal circuits
- Activation of fibrinolytic, fibrinogenolytic, and inflammatory pathways
- Hypothermia
- Anticoagulant use
- Platelet inhibitor use
- Congenital coagulopathies
Interplay between coagulation, anticoagulation and fibrinolytic system
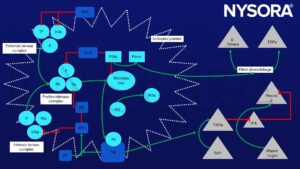
TF, Tissue Factor; PC, Protein C; PS, Protein S; TFPI(a), Tissue-Factor Pathway Inhibitor (activated); ATIII, Antithrombin III; FGN, Fibrinogen; TM, thrombomodulin; FDPs, Fibrin Degradation Products; tPA, tissue-Plasminogen Activator
Coagulation:
- Factors Xa and Va convert prothrombin to thrombin through the activation of factor X via intrinsic (factor IXa, VIIIa) and extrinsic tenase (Xase complexes)
- Thrombin cleaves fibrinogen into fibrin
- Fibrin polymerization is facilitated by the activation of factor XIII which forms cross-links leading to clot stabilization
- Prothrombin complex concentrate (PCC) administration targets factors II, VII, IX, and X for repletion
- Factor VIIa is targeted for repletion with the administration of recombinant factor VIIa (rFVIIa)
Anticoagulation:
- Anticoagulants negatively modulate clot formation
- Antithrombin III (ATIII) modulates factor IIa (primarily) and factor Xa (secondarily)
- ATIII-dependent inhibition of factor IXa, XIa, and VIIa-TFcomplex occurs to a lesser extent
- Other important anticoagulants include TFPI-modulation of Tissue Factor and factor VIIa, and Activated Protein C (APC)
- APC activates protein S and inhibits factor Va, weakening the prothrombinase complex and impairing thrombin generation
- Upstream, APC inhibits factor VIIIa of the intrinsic Xase complex
- Factor IIa complexes with Thrombomodulin (TM) to activate PC
- This complex initiates thrombin-activatable fibrinolysis inhibitor (TAFI), which prevents plasmin production
- Plasmin is the primary driver of fibrinolysis and results:
- In clot destabilization
- Degradation of fibrin cross-linkage
- Production of fibrin degradation products (D-dimers)
- Plasmin triggers platelet activation thereby competing with TAFI at the local level
Preoperative optimization
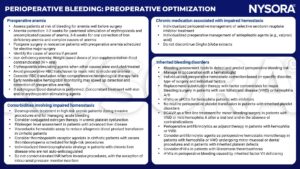
RBC, red blood cell; rFVIIa, recombinant activated factor VII; aPCC, activated prothrombin complex concentrate; DDAVP, desmopressin
NSAID, non-steroidal anti-inflammatory drug; LMWH, low molecular weight heparin; INR, international normalized ratio; PCC, prothrombin complex concentrate
COVID-19 coagulopathy
- Avoid major elective surgery in patients with COVID-19 coagulopathy
- In (semi)urgent surgery in patients with COVID-19 coagulopathy, avoid prophylactic TXA administration
- VHA-guided, goal-directed procoagulant treatment of perioperatively acquired coagulopathic bleeding avoiding overcorrection
- Perioperative drug monitoring of LMWH used as a standard anticoagulant in COVID-19 critical illness; If anti-Xa activity > 0.3 IU/mL in clinical bleeding, consider reversal with protamine
- A restrictive red blood cell transfusion strategy as in non-COVID-19 patients
- In patients recovered from COVID-19 and free of post-COVID-19 symptoms, manage severe perioperative bleeding as in non-COVID-19 patients
- Administer postoperative thromboprophylaxis as early as possible
- A restrictive red blood cell, plasma, and platelet transfusion strategy in the critically ill
- Use f a goal-directed coagulation therapy algorithm in the presence of ongoing bleeding, considering altered laboratory tests and VHA in critical illness
- If ongoing bleeding is unresponsive to multimodal coagulation therapy or there are wound healing defects in the critically ill, monitor FXIII and correct deficiency
- A restrictive systemic administration of TXA in case of fibrinolytic shutdown in critical illness
- Initiate thromboprophylaxis after bleeding as soon as the bleeding risk is overbalanced by the risk of thromboembolic complications
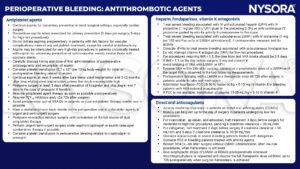
Perioperative bleeding control
- Perioperative bleeding is a major complication during and after surgery
- Massive transfusion protocols MTPs
- Defined as receiving ≥ 10 or more red blood cell units in 24h
- Include blood components or whole blood + coagulation factor concentrates, prothrombin complex concentrates (PCCs), and fibrinogen
- Bleeding management is guided by coagulation monitoring:
- Conventional coagulation tests: platelet counts, prothrombin time, and fibrinogen level
- Viscoelastic testing (VET)
- Hemostatic support is used to optimize hemostasis
- Surgical correction of site-specific bleeding
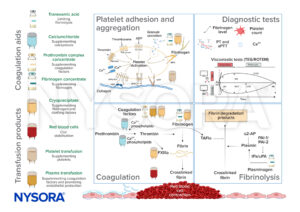
Fibrinogen
- A critical hemostatic factor for clot formation
- Converted into insoluble fibrin by thrombin and cross-linked by factor XIII
- Replete fibrinogen to a level of 1.5-2 g/L during bleeding using fibrinogen concentrates or cryoprecipitate
Ionized calcium
- Critical for coagulation
- Rapid infusion of citrated blood products administered during MTPs acutely lowers ionized calcium and inhibits calcium-dependent coagulation factors
- Maintain normocalcemia during resuscitation
PCCs and factor concentrates
- PCCs contain factors II, VII, IX, and X and variable levels of protein C, S, and antithrombin
- Developed for vitamin K antagonist reversal
- Increasingly used for perioperative bleeding management to correct perioperative coagulopathy
- Be aware of the potential thrombotic risks
- Other factor concentrates include recombinant FVIIa and factor XIII
Tranexamic acid (TXA)
- Routinely administered
- Early administration is beneficial in severely injured patients
- Consider the potential for increased thromboembolic risk in severe traumatic brain injury and gastrointestinal bleeding
Plasma transfusion
- Contains fresh-frozen plasma (FFP) or solvent-detergent plasma (SDP)
- Plasma does not correct clotting times
- May minimize endothelially during massive volume resuscitation
- Note that plasma transfusion is associated with TRALI, circulatory overload, bacterial contamination, and hypersensitivity reactions
Platelets
- Critical for hemostasis
- Red blood cells (RBCs) are initially administered in MTPs, followed by plasma and platelets
- Consider the use of cold-stored platelets as they have extended storage times
Red blood cells (RBCs)
- Change into a polyhedral shape when incorporated into a forming clot to maximize clot strength
- Interact with platelets, fibrinogen, von Willebrand factor, and FXIII to optimize clot formation
Coagulation support
- The goal of coagulation support during perioperative bleeding management is to promote clot formation
- Components of primary clot formation:
- Fibrinogen
- Fibrinogen concentrate
- Cryoprecipitate (contains more FXIII than most of the fibrinogen concentrates)
- Platelets: supplemented by platelet transfusion and activated by calcium supplementation
- Secondary coagulation process: promotion of thrombin and fibrin formation to further stabilize clot formation
- Calcium
- Plasma transfusion
- Prothrombin complex concentrate administration
- Coagulation process:
- By thrombin-activated FXIII crosslinks fibrin monomers to create a fibrin polymer network
- Red blood cells change their shape to further empower the stabilization of the clot
- Plasma transfusion, next to coagulation factor supplementation, also protects glycocalyx release and limits excessive clot formation
- Tranexamic acid binds lysine groups of plasminogen to limit the transversion of plasminogen into plasmin to reduce the fibrinolysis reaction
Coagulation support in perioperative bleeding management
Transfusion protocol
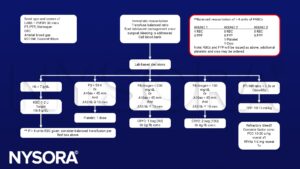
Inside the red box, our balanced ratio recommendations are presented if the patient has been transfused four units of blood and intraoperative hemorrhage is ongoing. CBC, complete blood count; Cryo, cryoprecipitate; FFP, fresh frozen plasma; Hgb, haemo-globin; RBC, red blood cell; PLT, platelet count; T & S, type and screen; PCC, prothrombin complex concentrates
Management
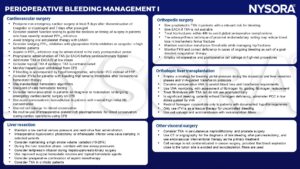
LMWH, low molecular weight heparin; TXA, tranexamic acid; EACA, epsilon-aminocaproic acid; CPB, Cardiopulmonary bypass; Hb, hemoglobin; PCC, prothrombin complex concentrate; FFP, fresh frozen plasma; rFVIIa, recombinant activated factor VII; FXIII, factor XIII; VHA, viscoelastic hemostatic assay
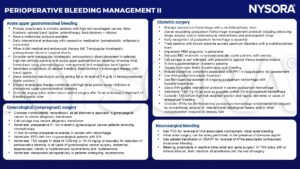
Hb, hemoglobin; EPO; erythropoietin; IDA, iron deficiency anemia; TXA, tranexamic acid; PBM, patient blood management; RBC, red blood cell; PPH, peripartum hemorrhage; VHA, viscoelastic hemostatic assay; rFVIIa, recombinant activated factor VII; PCC, prothrombin complex concentrate; DDAVP, desmopressin
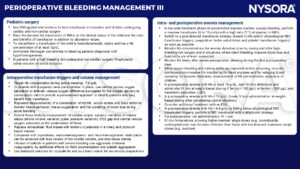
VHA, viscoelastic hemostatic assay; RBC, red blood cell; Hb, hemoglobin; Hct, hematocrit; ESA, erythropoietin-stimulating agent
Suggested reading
- Kietaibl S, Ahmed A, Afshari A, Albaladejo P, Aldecoa C, Barauskas G, et al. Management of severe peri-operative bleeding: Guidelines from the European Society of Anaesthesiology and Intensive Care: Second update 2022. European Journal of Anaesthesiology | EJA. 2023;40(4).
- Ghadimi K, Levy JH, Welsby IJ. Perioperative management of the bleeding patient. Br J Anaesth. 2016;117(suppl 3):iii18-iii30.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







