Learning objectives
- Stages of HIV
- Progression to AIDS
- Anesthetic management of HIV and AIDS
Definition and mechanisms
- HIV (human immunodeficiency virus) is a virus that attacks the body’s immune system, making a person more vulnerable to other infections and diseases
- If HIV is not treated, it can lead to AIDS (acquired immunodeficiency syndrome)
- Effective treatment with antiretroviral therapy to reduce the viral load is available, however, no cure exists
- AIDS is the late stage of HIV infection that occurs when the body’s immune system is badly damaged because of the virus
Signs and symptoms
- Flu-like symptoms within 2-4 weeks after injection
- Fever
- Headache
- Diarrhea
- Weight loss
- Cough
- Sore throat
- Swollen lymph nodes
- Rash
- Muscle aches
- Night sweats
- Mouth ulcers
- Fatigue
Stages of HIV
| Stage 1: acute HIV infection | Stage 2: chronic or clinical latent HIV infection | Stage 3: acquired Immunodeficiency Syndrome (AIDS) |
|---|---|---|
| A large amount of HIV in the blood which is very contagious Flu-like symptoms | Asymptomatic HIV infection or clinical latency HIV is still active and continues to reproduce Patients may not have any symptoms but can still transmit HIV Intake of HIV treatment can prevent the development of stage 3 (AIDS) At the end of this stage, the HIV viral load increases, and the patient moves into stage 3 (AIDS) | The most severe stage of HIV infection High viral load and may easily transmit HIV to other people Opportunistic infections or other serious illnesses People with AIDS typically survive about three years without HIV treatment |
| A person with HIV is considered to have progressed to AIDS when: The number of their CD4 cells falls below 200 cells per cubic millimeter of blood (200 cells/mm3) OR they develop one or more opportunistic infections regardless of their CD4 count |
Major opportunistic pathogens in HIV/AIDS
| Protozoa | Pnemocystis carinii Toxoplasma gondii Cryptosporidium parvum Microsporidia spp. Isospora belli |
| Fungi and yeasts | Candida spp. Cryptococcus neoformans Histoplasma capsulatum Coccidioides immitis |
| Viruses | Cytomegalovirus Herpes simplex Varicella zoster |
| Bacteria | Mycobacterium avium intracellulare Mycobacterium tuberculosis Streptococcus pneumoniae Haemophillus influenzae Salmonella spp. Nocardia Moraxella catarrhalis |
Treatment
- Highly active antiretroviral therapy (HAART) to slow the progression of the disease
- Combination or cocktail of antiretroviral agents to prevent resistance to the virus, typically:
- a non-nucleoside reverse transcriptase inhibitor (NNRTI)
- Two nucleoside analog reverse transcriptase inhibitors (NRTIs)
- Consider side effects of antiretrovirals:
- Bone marrow suppression
- Renal failure
- Peripheral neuropathy
- p450 activation
- Lactic acidosis
- Insulin resistance
- Dyslipidemia
- Treatment of opportunistic infection
Management
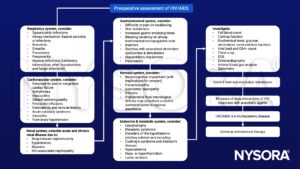
Preoperative management
Intraoperative management
- Reduce the risk of cross infection
- Vigilance in the use of universal precautions
- Administer post-exposure prophylaxis (PEP) to healthcare workers as soon as possible after the injury, ideally within 1–2 hours
- Obstetric anesthesia
- Cesarean section reduces the incidence of mother-to-child transmission
- Administer ART
- RA is not contraindicated
- Epidural blood patch for PDPH is safe
- Pain management
- Multidisciplinary pain management
Suggested reading
- Leelanukrom R. Anaesthetic considerations of the HIV-infected patients. Curr Opin Anaesthesiol. 2009;22(3):412-418.
- Wilson, S. 2009 HIV and anaesthesia. Updtae in anaesthesia.
- Prout J, Agarwal B. 2005. Anaesthesia and critical care for patients with HIV infection. Continuing Education in Anaesthesia Critical Care & Pain. 5;5:153–156.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com