Learning objectives
- Types of spina bifida
- Perioperative management of spina bifida
Definition and mechanism
- Refers to a congenital neural tube defect
- Results from the failure of the fetal neural tube to close within the first three weeks of gestation
- This leads to the incomplete fusion of the posterior lamina and pines of the vertebral column, and most commonly in the lumbosacral segments
- The incidence is approximately 1:1000 live births, however, the incidence is decreasing due to folate supplementation
- Often no symptoms and often discovered as an incidental finding on radiographic examination
- Dimpling of the skin or a hairy patch at the base of the spine may be present in up to 70% of the patients with cord abnormalities
Types of spina bifida
| Spina bifida occulta (closed spina bifida) | Meningocele | Myelomeningocele |
|---|---|---|
| The most common and mildest type A midline defect of the spinal column without protrusion of the spinal cord or meninges and intact overlying skin No associated hydrocephalus or hindbrain herniation One or more vertebrae do not form properly, but the gap is very small Most affected individuals are asymptomatic and lack neurological signs In some cases, it may be associated with patches of hair, a lipoma, discoloration of the skin, or a dermal sinus in the midline of the low back | The least common form of spina bifida A single developmental defect allows the meninges to herniate between the vertebrae But the spinal cord assumes a normal position in the spinal canal Cases of tethered cord have been reported | Various amounts of neural tissue and meninges herniate through the defect to form a cerebrospinal fluid (CSF)-filled sac structure covered by a thin layer of skin tissue May rupture and leak cerebrospinal fluid The extent of the neurological deficit depends greatly on the location of the meningomyelocele, it most commonly occurs in the lumbosacral region Clinical features: - Flaccid paralysis of the lower limbs, absence of deep tendon reflexes, lack of response to touch and pain, kyphosis, scoliosis, and urinary and fecal incontinence - Postural abnormalities of the lower limbs including clubfeet and subluxation of the hip - Lesions above T4 generally result in paraplegia, whereas lesions below S1 allow ambulation Associated with hydrocephalus and type II Arnold-Chiari malformation Hydrocephalus is typically managed with a ventriculoperitoneal shunt |
Risk factors
- Lack of folic acid before and in the early stages of pregnancy
- Family history of spina bifida
- Medication intake during pregnancy: valproic acid, calcium-channel blockers, carbamazepine, cytochalasins
Conditions associated with spina bifida
- Attention and learning difficulties
- Bladder function problems
- Bowel function problems
- Depression
- Epilepsy and seizures
- Hip displacement
- Hydrocephalus
- Latex allergy
- Vision problems
- Lymphedema
- Obesity
- Pressure injury
- Scoliosis
- Sleep apnea
- Tethered spinal cord
- Weakness or paralysis
Diagnosis
- X-ray
- CT and MRI
Prenatal diagnosis
- Ultrasound
- Detection of alpha-fetoprotein in amniotic fluid
Management
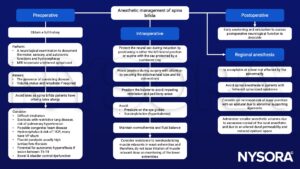
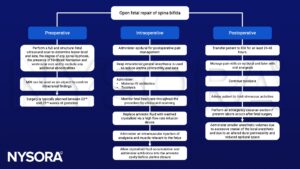
Pregnancy
- Neuraxial is generally safe
- Consider:
- Difficulty locating the epidural space
- An asymmetric block likely related to scarring
- Dural punctures
- The need for multiple operator attempts to place the anesthesia
- A higher risk of post dural puncture headache
- The conus medullaris will likely be in an abnormal low position
- Scoliosis can further complicate the spine anatomy
- Use imaging to locate the best level for neuraxial anesthesia
- Attempt a block at the level where the cord is not too posteriorly located and the epidural space is likely to be normal
- Meningocele & myelomeningocele:
- If spinal level involvement T11 or higher, likely will have painless labor
Open surgery
Suggested reading
- Sacco, A., Ushakov, F., Thompson, D., Peebles, D., Pandya, P., De Coppi, P., Wimalasundera, R., Attilakos, G., David, A.L., Deprest, J., 2019. Fetal surgery for open spina bifida. The Obstetrician & Gynaecologist 21, 271–282.
- O’Neal MA. A Pregnant Woman with Spina Bifida: Need for a Multidisciplinary Labor Plan. Front Med (Lausanne). 2017;4:172.
- Griffiths, S., Durbridge, J.A., 2011. Anaesthetic implications of neurological disease in pregnancy. Continuing Education in Anaesthesia Critical Care & Pain 11, 157–161.
- Spina Bifida. In: Bissonnette B, Luginbuehl I, Marciniak B, Dalens BJ. eds. Syndromes: Rapid Recognition and Perioperative Implications. McGraw Hill; 2006.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com