Learning objectives
- Define umbilical cord prolapse
- Describe the risk factors for developing umbilical cord prolapse
- Umbilical cord prolapse management
Definition and mechanisms
- Umbilical cord prolapse is an obstetric emergency in which the umbilical cord descends through the cervix alongside (occult) or past (overt) the fetal presenting part
- It can occur before or during the delivery of the baby, usually close to the end of pregnancy (after 37 weeks)
- Compression of, or vasospasm of, the umbilical cord impairs the blood flow between the placenta and fetus, leading to fetal hypoxia and bradycardia
- Fetal hypoxia may result in fetal death or permanent disability if not rapidly diagnosed and managed
- Early recognition and intervention are important to reduce the adverse outcomes in the fetus
Classification
- Overt prolapse: Cord exits the cervix before the fetal presenting part
- Occult prolapse: Cord exits the cervix with the fetal presenting part
Complications
- Surviving infants may develop complications secondary to asphyxia (i.e., neonatal encephalopathy and cerebral palsy)
- Stillbirth
Risk factors
- Maternal age ≥35 years
- Premature rupture of membranes
- Preterm delivery
- Low birth weight
- Multiple gestation pregnancies
- Placenta praevia
- Polyhydramnios
- Fetal malpresentation (i.e., breech presentation)
- External cephalic version procedure
- Intrauterine growth restriction
- Fetal and cord abnormalities
Diagnosis
- Fetal bradycardia (<120 bpm) in the setting of ruptured membranes should prompt immediate evaluation for potential cord prolapse
- Umbilical cord prolapse is diagnosed by seeing or palpating the prolapsed cord on pelvic examination
| Overt prolapse | Occult prolapse |
|---|---|
| Diagnosis is clinical and made by palpation of a pulsating structure in the vaginal vault or visibly protruding from the vaginal introitus Typically accompanied by fetal bradycardia or severe variable decelerations | Only fetal bradycardia may appear The cord is not visible or palpable ahead of the fetal presenting part |
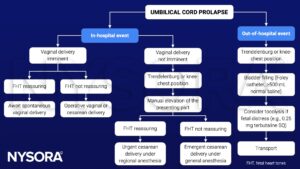
Management
Goal: Avoid cord compression and vasospasm
- Call for help
- Establish an intravenous line (if not already placed)
- Ensure continuous fetal monitoring
- Administer oxygen via a face mask (if needed)
- Administer aspiration prophylaxis
- Umbilical cord prolapse is an acute obstetric emergency requiring immediate delivery of the baby, usually via cesarean section
- Allow instrumental/vaginal delivery if considered quicker
- Inform the anesthesiologist, pediatrician, and OR staff
- Patient consent
- Funic decompression: Elevating the fetal presenting part to aid cord decompression
- Two fingers/hand in the vagina – manual elevation of the presenting part
- Steep Trendelenburg or knee-chest position, lying on the left side is preferred
- Bladder filling with a Foley catheter (≥500 mL of normal saline)
- Funic reduction (rarely used): Replacement of the umbilical cord into the uterus
- Tocolysis in case of fetal distress or if prolonged interval to delivery is expected
- Keep the cord warm and moist if it is protruding from the vagina and delivery is not imminent
- Avoid aortocaval compression
- Minimize handling of the cord outside of the vagina to prevent vasospasm
See also cesarean section considerations
Suggested reading
- Boushra M, Stone A, Rathbun KM. Umbilical Cord Prolapse. [Updated 2022 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542241/
- Sayed Ahmed WA, Hamdy MA. Optimal management of umbilical cord prolapse. Int J Womens Health. 2018;10:459-465.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com