Learning objectives
- Describe cerebral palsy
- Recognize the symptoms and signs of cerebral palsy
- Outline the anticipated challenges for airway management in patients with cerebral palsy
- Identify common intraoperative complications associated with cerebral palsy
Definition and mechanisms
- Cerebral palsy (CP) is a group of permanent neurodevelopmental disorders that affects an individual’s muscle tone, motor functions, movement, and posture
- CP is attributed to non-progressive disturbances that occur in the developing fetal or infant brain
- CP is the most common motor disability in childhood
Signs and symptoms
- Signs and symptoms vary among people
- CP can affect the whole body or might be limited primarily to one or two limbs, or one side of the body
- Symptoms get more noticeable over the first few years of life, but underlying problems do not worsen over time
Movement and coordination
- Stiff muscles and exaggerated reflexes (spasticity)
- Variations in muscle tone (too stiff or floppy)
- Stiff muscles with normal reflexes (rigidity)
- Lack of balance and muscle coordination (ataxia)
- Tremors or jerky involuntary movements
- Favoring one side of the body (e.g., only reaching with one hand or dragging a leg while crawling)
- Difficulty walking (e.g., walking on toes, crouched gait, scissors-like gait with knees crossing, wide gait, or asymmetrical gait)
- Difficulty with fine motor skills
Speech and eating
- Delays in speech development
- Difficulty speaking
- Difficulty with sucking, chewing, or eating
- Excessive drooling or problems with swallowing
Development
- Delays in reaching motor skills milestones (babies with CP do not roll over, sit, crawl, or walk as early as other children of their age)
- Learning disability
- Intellectual disability
- Delayed growth (smaller size than expected)
Other problems
- Epilepsy
- Difficulty hearing
- Problems with vision and abnormal eye movements
- Abnormal touch or pain sensations
- Bladder and bowel problems (e.g., constipation and urinary incontinence)
- Mental health conditions (e.g., emotional disorders and behavioral problems)
Risk factors
Congenital CP (80%)
- Fetal pathogenic factors
- Vascular maldevelopments
- Congenital genetic/metabolic disorders
- Microcephaly
- Fetal trauma
- Neonatal asphyxia in the peripartum period (6%)
- Low birth weight (<2.5 kg)
- Prematurity (<32 weeks)
- Low Apgar score
- Multiple births
- Prenatal “TORCH” infections (toxoplasmosis, rubella, cytomegalovirus, and herpes)
- Maternal pathogenic factors
- Breech presentation
- Pre-eclampsia
- Peripartum hemorrhage
- Maternal hyperthyroidism
- Fetal alcohol syndrome
Acquired CP (20%) → develops during the first 2 years of life
- Intracerebral hemorrhage
- Viral encephalitis
- Bacterial meningitis
- Hyperbilirubinemia (kernicterus)
- Head injury
- Neonatal seizures
Complications
Muscle weakness, muscle spasticity, and coordination problems may contribute to complications during childhood or adulthood
- Contracture: Muscle tissue shortening due to severe muscle tightening as a result of spasticity → can inhibit bone growth, cause bones to bend, and result in joint deformities, dislocation, or partial dislocation (e.g., hip dislocation, scoliosis)
- Malnutrition: Swallowing or feeding problems limit the infant to get enough nutrition → impair growth and weaken bones
- Mental health conditions: Depression and behavioral problems
- Cardiopulmonary disease
- Increased risk of aspiration pneumonitis and subsequent chronic lung scarring due to swallowing difficulties, esophageal dysmotility, abnormal lower esophageal sphincter tone, and spinal deformity → gastroesophageal reflux disease (GERD)
- Decreased immunity, poor nutrition, respiratory muscle hypotonia, and a weak cough in conjunction with GERD make patients more susceptible to recurrent chest infections, exacerbating the underlying chronic lung disease
- Long-term truncal muscle spasticity can lead to scoliosis, restrictive lung defects, pulmonary hypertension, and ultimately cor pulmonale and respiratory failure
- Osteoarthritis: Pressure on joints or abnormal alignment of joints from muscle spasticity may lead to the early onset of osteoarthritis
- Osteoporosis: Fractures due to low bone density resulting from lack of mobility, inadequate nutrition, and anti-epileptic drug use
- Other complications: Sleep disorders, chronic pain, skin breakdown, intestinal problems, and issues with oral health
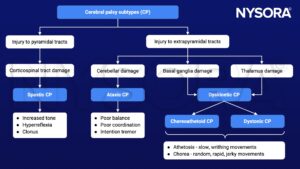
Pathophysiology

Treatment
Treatment is focused on
- Improving posture and mobility by reducing spasticity, muscle spasms, and contractures
- Symptomatic relief of the associated medical problems (e.g., epilepsy, GERD, chest infections)
Combination therapies are more successful than single-treatment protocols: Physiotherapy, psychological counseling, occupational, speech, and behavioral therapy combined with
- Antispastic medications (e.g., baclofen)
- Neuromuscular denervation techniques (e.g., botulinum toxin injections, radiofrequency ablation of dorsal horn ganglia, and dorsal rhizotomy)
- Surgery (e.g., tenotomies, arthrodeses, osteotomies tendon transfer/lengthening, and multisegmental spinal fusion procedures)
Management
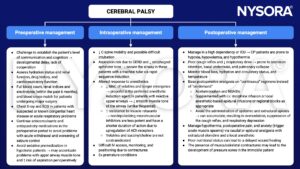
Keep in mind
- CP describes a spectrum of movement and posture disorders resulting from pathological injury to the developing fetal or infant brain
- Commonly associated comorbidities include dehydration, malnutrition, epilepsy, GERD, and impaired lung function
- Frequently encountered perioperative problems include difficulties with patient positioning and vascular access
- Regional analgesic techniques to reduce postoperative pain, muscle spasms, and respiratory complications are beneficial
Suggested reading
- Prosser DP, Sharma N. Cerebral palsy and anaesthesia. Continuing Education in Anaesthesia Critical Care & Pain. 2010;10(3):72-76.
- Miller B, Rondeau B. Anesthetic Considerations In Patients With Cerebral Palsy. [Updated 2022 Jun 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572057/
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com