Learning objectives
- Define tetralogy of Fallot
- Describe the signs and symptoms of tetralogy of Fallot
- Understand the pathophysiology of tetralogy of Fallot
- Anesthetic management of a patient with tetralogy of Fallot
Definition and mechanisms
- Tetralogy of Fallot (TOF) is one of the most congenital heart defects (10%), resulting in a right-to-left shunt characterized by
- Large non-restrictive ventricular septal defect (VSD)
- Valvular, subvalvular, or supravalvular pulmonary stenosis, causing right ventricular outflow tract obstruction (RVOTO)
- Right ventricular hypertrophy
- Overriding aorta
- Cyanotic heart disease
- TOF often presents with low birth weight and prematurity
- TOF may present with other anatomical anomalies
- Stenosis of the left pulmonary artery (40%)
- Bicuspid pulmonary valve (60%)
- Right-sided aortic arch (25%)
- Coronary artery anomalies (10%)
- Patent foramen ovale or atrial septal defect → pentalogy of Fallot
- Atrioventricular septal defect
- Partially or totally anomalous pulmonary venous return
Signs and symptoms
- Right-to-left shunt
- Cyanosis (bluish coloration of the skin caused by hypoxemia)
- Hypoxia/low SpO2 (60-90%) with little or no response to oxygen therapy
- Shortness of breath and rapid breathing, especially during feeding or exercise
- Heart murmurs (pansystolic and ejection systolic)
- Abnormal, rounded shape of the nail bed in the fingers and toes (clubbing)
- Poor weight gain
- Tiring easily during feeding or exercise
- Irritability
- Prolonged crying
- Polycythemia
- Baby may turn blue with breastfeeding or crying
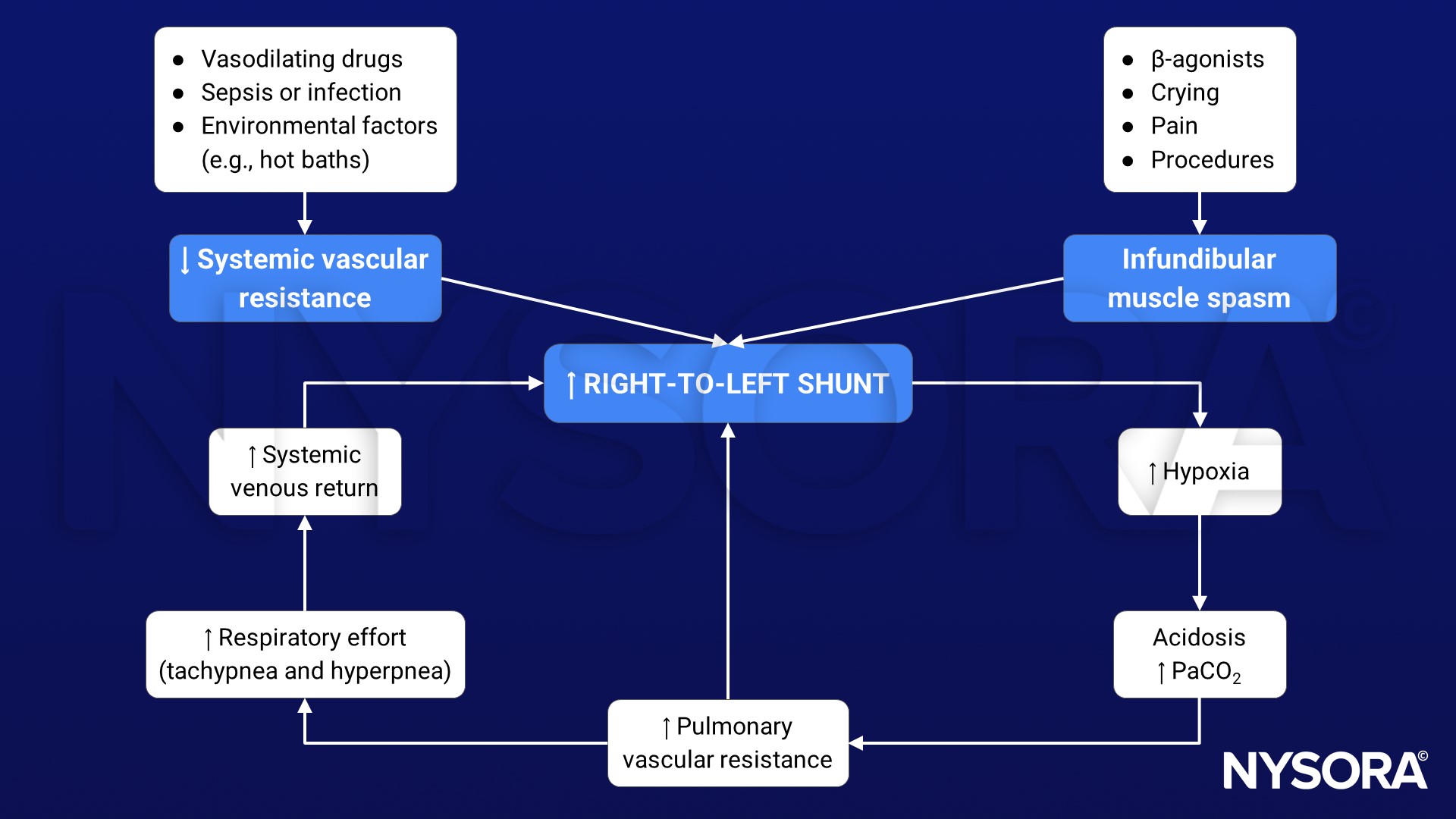
Tet spells
- Infants and children with unrepaired TOF may develop tet spells → acute hypoxia spells, characterized by shortness of breath, cyanosis, agitation, and loss of consciousness (syncope)
- Initiated by any event (i.e., crying, bowel movements, anxiety, pain, dehydration, or fever) that leads to decreased oxygen saturation or that causes decreased systemic vascular resistance (SVR) → increased shunting through the VSD (increased right-to-left shunt)
- Decrease in frequency after the first four years of life
- Older children will squat to increase the SVR → temporary reversal of shunt
Complications
- Endocarditis
- Arrhythmias (particularly supraventricular or ventricular)
- Pulmonary regurgitation
- Dizziness, fainting, or seizures due to hypoxemia
- Delayed growth and development
Risk factors
- Viral illness during pregnancy (rubella)
- Maternal alcohol consumption
- Maternal smoking
- Maternal diabetes mellitus or gestational diabetes
- Maternal age >40
- Family history of TOF
- Down syndrome or DiGeorge syndrome
- Tracheoesophageal fistula or VACTERL association
- Male gender
Pathophysiology
Anatomy of TOF allows mixing of blood between the pulmonary and systemic circulations (usually at VSD) → right-to-left shunt adding deoxygenated blood to the systemic circulation → cyanosis
Diagnosis
- Many patients are diagnosed prenatally
- Chest radiography: Abnormal “coeur-en-sabot” (boot-like) appearance of the heart
- Electrocardiogram: Right ventricular hypertrophy along (tall R-waves in lead V1 and deep S-waves in lead V5-V6) with right-axis deviation
- Echocardiogram: Presence of VSD, right ventricular hypertrophy, and aortic override; color Doppler to measure the degree of pulmonary stenosis
Treatment
- Surgical repair
- Patch closure of the VSD to separate the pulmonary and systemic circulation
- Enlargement of the RVOT (increase the size of the pulmonary valve and pulmonary arteries) to relieve RVOTO
- Usually takes place in the first year following birth, at age 3-6 months
- Intraoperative transesophageal echo to evaluate the VSD closure and RVOT
Long-term complications after TOF surgery
- Chronic pulmonary valve regurgitation
- Tricuspid valve regurgitation
- VSD that may continue to leak after repair or may need re-repair
- Hypertrophic right or left ventricle and dysfunction
- Arrhythmias
- Coronary artery disease
- Aortic root and valve dilation
- Sudden cardiac death
Management
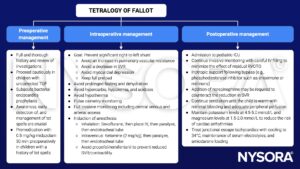
Management of tet spells during anesthesia
- Goal: Increase oxygenation, improve cardiac output, and reduce infundibular spasm and right-to-left shunt
- Give 100% oxygen and check the endotracheal tube position
- Deepen anesthesia and give an opiate bolus (e.g., 0.1 mg/kg morphine)
- Fluid bolus
- Vasopressor therapy (e.g., 5 mcg/kg phenylephrine)
- β-blockers (e.g., 0.1-0.3 mg/kg propranolol)
- Knee-to-chest flexion position
Keep in mind
- TOF is characterized by the presence of a VSD, RVOTO, right ventricular hypertrophy, and overriding aorta
- TOF is one of the most common cyanotic heart defects
- Prevention of tet spells is the key for safe anesthesia
Suggested reading
- Wilson R, Ross O, Griksaitis MJ. Tetralogy of Fallot. BJA Educ. 2019;19(11):362-369.
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 2 Cardiovascular system, Tully RP and Turner R.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







