Learning objectives
- Recognize common causes of TR
- Describe the signs and symptoms of TR
- Grade the severity of TR cases
- Anesthetic management of TR
Definition & mechanisms
- Tricuspid regurgitation (TR) occurs when the tricuspid valve does not close properly, causing a reversal of blood flow through the valve
- TR can be of primary or secondary origin:
- Primary (organic) TR: Pathology of the tricuspid valve complex, may be of rheumatic, degenerative, congenital, infectious, traumatic, or iatrogenic origin
- Secondary (functional) TR: Related to right ventricular dilatation and/or dysfunction, annular dilatation, and leaflet tethering, usually secondary to left-sided valvular heart disease, atrial fibrillation or pulmonary hypertension
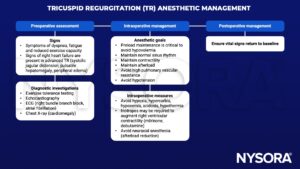
Signs & symptoms
- Often clinically silent and symptoms usually relate to concomitant left-sided valvular heart disease
- General fatigue and reduced exercise capacity
- Upper abdominal pain
- Peripheral lower limb edema
- Systolic jugular distension
- Pulsatile hepatomegaly
- Ascites, liver failure, and cachexia may be observed in end-stage disease
- Electrocardiogram frequently shows right bundle branch block and atrial fibrillation reflects disease evolution.
Severity assessment
| Parameters | Mild | Moderate | Severe | |
|---|---|---|---|---|
| Qualitative | TV morphology | Normal/abnormal | Normal/abnormal | Abnormal/flail/large coaptation defect |
| Color flow TR jet | Small, central | Intermediate | Very large central jet or eccentric wall impinging jet | |
| CW signal of TR jet | Faint/parabolic | Dense/parabolic | Dense/triangular with early peaking (peak <2 m/s in massive TR) | |
| Semi-quantitative | VC width (mm) | Not defined | <7 | >7 |
| PISA radius (mm) | ≤5 | 6–9 | >9 | |
| Hepatic vein flow | Systolic dominance | Systolic blunting | Systolic flow reversal | |
| Tricuspid inflow | Normal | Normal | E-wave dominant (≥1 m/s) | |
| Quantitative | EROA (mm2) | Not defined | Not defined | ≥40 |
| R Vol (ml) | Not defined | Not defined | ≥45 |
Management
Keep in mind
Tricuspid regurgitation is most commonly secondary to other morbidities, which might require further attention.
Suggested reading
- Antunes MJ, Rodríguez-Palomares J, Prendergast B, De Bonis M, Rosenhek R, Al-Attar N, et al. Management of tricuspid valve regurgitation: Position statement of the European Society of Cardiology Working Groups of Cardiovascular Surgery and Valvular Heart Disease. European Journal of Cardio-Thoracic Surgery. 2017;52(6):1022-30.
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com