Learning objectives
- Define DiGeorge syndrome
- Describe the signs, symptoms, and complications associated with DiGeorge syndrome
- Anesthetic management of a patient with DiGeorge syndrome
Definition and mechanisms
- DiGeorge syndrome, or 22q11.2 deletion syndrome, is a syndrome caused by a heterozygous microdeletion on the long arm of chromosome 22
- This deletion results in the poor development of several body systems
- 90% of cases occur due to a new mutation during early development, while 10% are inherited (autosomal dominant)
- Memory aid: CATCH-22
- Cyanotic congenital heart defect
- Abnormal facies
- Thymic aplasia or hypoplasia
- Cognitive impairment, cleft palate
- Hypoparathyroidism, hypocalcemia
- 22q11.2 deletion
Signs, symptoms, and complications
- Congenital heart disease (40%): Particularly conotruncal malformations (e.g., interrupted aortic arch, persistent truncus arteriosus, tetralogy of Fallot, and ventricular septal defect)
- Cyanosis
- Palatal abnormalities (50%): Velopharyngeal incompetence, submucosal cleft palate, and cleft palate with or without cleft lip
- Characteristic facial features (including hypertelorism): Underdeveloped chin (micrognathia and retrognathia), low-set ears, wide-set eyes, or a narrow groove in the upper lip
- Frequent infections due to thymic aplasia or hypoplasia
- Developmental delay
- Learning difficulties (90%) including cognitive deficits, attention deficit disorders
- Hypocalcemia (50%) due to hypoparathyroidism
- Significant feeding problems (30%), gastroesophageal reflux disease (GERD), and failure to thrive
- Renal anomalies (37%)
- Hearing loss
- Laryngotracheoesophageal anomalies
- Growth hormone deficiency
- Autoimmune disorders (e.g., rheumatoid arthritis or Graves disease)
- Immune disorders due to reduced T-cell numbers
- Seizures (with or without hypocalcemia)
- Skeletal abnormalities (e.g., scoliosis)
- Psychiatric disorders and behavioral problems (e.g., schizophrenia develops in 25-30% by adulthood, ADHD, autism spectrum disorder)
Pathophysiology

Treatment
There is no cure for DiGeorge syndrome, but certain individual features are treatable using standard treatments
- Hypoparathyroidism: Calcium and vitamin D supplements
- Congenital heart defects: Surgical repair soon after birth to repair the defect and improve the supply of oxygen-rich blood
- Limited thymus gland function: Infections (e.g., colds and ear infections) are generally treated as they would be in any child; normal schedule of vaccines
- Severe thymus gland function: Transplant of thymus tissue, specialized bone marrow, or specialized disease-fighting blood cells
- Cleft palate: Surgical repair
- Overall development: Speech therapy, occupational therapy, and developmental therapy
Anesthesia considerations
- Airway
- Difficult airway
- Small mouth opening, retrognathia, micrognathia
- Cleft palate, velopharyngeal insufficiency: Avoid nasal intubation
- Aspiration risk
- Pharyngeal insufficiency, GERD
- Difficult airway
- Breathing
- Nasal obstruction
- Obstructive sleep apnea (OSA)
- Circulation
- Conotruncal anomalies
- Long QT from hypocalcemia
- Disability
- Developmental delay, behavioral issues
- Tetany and seizures from hypocalcemia
- Genitourinary
- Hypocalcemia from hypoparathyroidism (especially in newborns)
- Renal anomalies
- Immunodeficiency
- Thymic hypoplasia: Recurrent infections; aseptic technique needed
- Thymic aplasia: Severe combined immunodeficiency (SCID)
- Musculoskeletal
Management
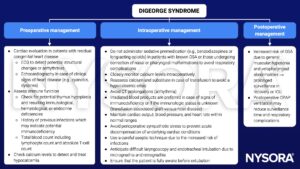
Keep in mind
- Perform a recent cardiac evaluation in patients with residual congenital heart disease
- Anticipate a difficult intubation
- Use a careful aseptic technique
- Check calcium levels
Suggested reading
- Haché M. DIGEORGE SYNDROME. In: Houck PJ, Haché M, Sun LS. eds. Handbook of Pediatric Anesthesia. McGraw Hill; 2015. Accessed March 06, 2023. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=1189§ionid=70364073
We would love to hear from you. If you should detect any errors, email us [email protected]