Learning objectives
- Describe the causes and consequences of ASD
- Recognize risk factors for ASD
- Diagnose ASD
- Anesthetic management of patients with ASD
Definition & mechanisms
- Atrial septal defect (ASD) is one of the most common types of congenital heart defects, occurring in about 25% of children
- Failure to close the septum between the right and left atria
- Small defects usually close spontaneously during childhood
- Large defects that do not close spontaneously may require percutaneous or surgical intervention
- Blood flows from the left atrium to the right atrium causing a left-to-right shunt
- Increase in pulmonary vascular resistance due to chronic volume overload, resulting in pulmonary hypertension
- Once pulmonary pressures equal systemic pressures, the shunt across the ASD reverses, and deoxygenated blood flows into the left atrium and systemically (Eisenmenger syndrome)
- Other complications:
- Atrial dysrhythmias
- Right-sided congestive heart failure
- Transient ischemic attack/stroke
Risk factors
| Secondary to inherited disorder | Down syndrome |
| Treacher-Collins syndrome | |
| Thrombocytopenia-absent radii syndrome | |
| Turner syndrome | |
| Noonan syndrome | |
| Maternal exposures | Rubella |
| Alcohol | |
| Drugs, e.g., cocaine |
ASD types
- Ostium secundum defect: Increased reabsorption of the septum primum in the atrium’s roof, or the septum secundum does not occlude the ostium secundum
- Ostium primum defect: Failure of the septum primum to fuse with the endocardial cushions
- Sinus venosus defect: Superior and inferior defects occur, and neither involves the true membranous septum:
- Superior defect: The orifice of the superior vena cava overrides the atrial septum above the oval fossa and drains both the left and right atria
- Inferior defect: The orifice of the inferior vena cava overrides both atria
- Coronary sinus defect: A defect or hole in the common wall between the left atrium and the coronary sinus creates a communication between the right and left atria
Diagnosis
- Transthoracic echocardiogram (gold standard diagnostic imaging modality)
- Cardiac CT and MRI
- Exercise testing can help determine the reversibility of shunt flow and the response of patients with pulmonary artery hypertension to activity
- Cardiac catheterization is contraindicated in young patients who present with small, uncomplicated ASDs.
- Differential diagnosis:
- Atrioventricular septal defect
- Ventricular septal defect
- Cyanotic congenital heart disease (sinus venosus defects and coronary sinus defects)
- Total anomalous pulmonary venous return
- Pulmonary stenosis
- Truncus arteriosus
- Tricuspid atresia
Management
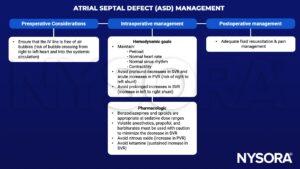
SVR, systemic vascular resistance; PVR, pulmonary vascular resistance
Suggested reading
- Menillo AM, Lee LS, Pearson-Shaver AL. Atrial Septal Defect. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535440/
- Yen P. ASD and VSD Flow Dynamics and Anesthetic Management. Anesth Prog. 2015;62(3):125-130.
- Calvert PA, Klein AA. Anaesthesia for percutaneous closure of atrial septal defects. Continuing Education in Anaesthesia Critical Care & Pain. 2008;8(1):16-20.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com