Learning objectives
- Define malnutrition
- Describe how malnutrition affects different body systems
- Anesthetic management of the malnourished patient
Definition and mechanisms
- Malnutrition or nutritional deficiency occurs when there is a negative balance between nutritional supply and demand
- Reduced supply states are caused by mechanical obstruction, poor absorption, and psychogenic eating disorders (e.g., anorexia nervosa)
- Increased demand occurs in hypermetabolic states (e.g., sepsis, trauma, and cancer)
- It is a deficiency, excess, or imbalance of energy, protein, and other nutrients, which adversely affects the body’s tissues and form
- Malnutrition occurs in approximately half of the surgical patients, resulting in an increased incidence of postoperative complications
- The main symptoms are unintentional weight loss (≥5-10% over 3-6 months) and a low body weight (BMI <18.5 kg/m2)
Note: Malnutrition involves both undernutrition and overnutrition, however, this article will only discuss undernutrition, for overnutrition the reader is referred to the obesity considerations
Signs and symptoms
Body systems affected by malnutrition
| System | Features |
|---|---|
| Central nervous system | Impaired mental ability Mental depression Depressed cognitive function Fatigue and generalized weakness |
| Musculoskeletal | Reduced muscle mass and strength Histologically confirmed myopathy in severe anorexia nervosa patients Reduced bone mass, osteopenia, and osteoporosis with secondary fractures Impaired thermoregulation Impaired wound healing |
| Cardiovascular | Reduction in cardiac output Hypotension and bradycardia Increased risk of arrhythmia due to vitamin and electrolyte disturbance Mitral valve prolapse Loss of cardiac muscle mass with associated reduced left ventricular function and ejection fraction Increased vagal tone Peripheral vasoconstriction Sinus arrest and wandering atrial pacemakers ECG changes: Prolonged QTc, ST depression and T-wave inversion |
| Respiratory | Reduced respiratory muscle strength and function Spontaneous pneumothorax Pneumomediastinum from persistent vomiting Decreased respiratory compliance (due to decreased elasticity of lung tissues) |
| Renal | Reduced glomerular filtration rate Total body water proportionally higher Proteinuria High urea due to dehydration |
| Gastrointestinal | Decreased enteral feeding leading to gut atrophy, bacterial translocation, and impaired immune function Esophagitis and Mallory-Weiss tear from purging Gastric dilatation Paradoxical decrease in gastric emptying time |
| Micronutrient disturbances | Vitamin A insufficiency - blindness (xerophthalmia due to corneal ulceration is the leading cause of childhood blindness), immunosuppression Reduced iron, ferritin, and iron deficiency anemia Low folic acid and zinc levels |
| Electrolyte disturbances | Hypokalemia (due to repeated purging and vomiting) Hypocalcemia (prolonged nondepolarizing muscle relaxation action) Hypoglycemia and hypoglycemic coma Metabolic alkalosis (more likely in patients who purge) Increased cortisol and corticotrophin-releasing hormone levels with blunted response |
| Hematological | Leucopenia Often normal immune function until 50% drop in normal expected body weight Elevated liver transaminases Anemia Pancytopenia |
| Pharmacological | Delayed or reduced absorption of drugs Hypoalbuminemia increases free fraction of drugs, decreased protein binding occurs Pseudocholinesterase deficiency in severe malnutrition (severe albumin <2 g/dL) → prolonged treatment with nondepolarizing muscle relaxants Lower total body mass means reduced drug doses required and lowered thresholds for toxicity Neostigmine, edrophinium, and catecholamines can cause life-threatening arrhythmias |
Risk factors
- Lack of breastfeeding
- Anorexia nervosa
- Bulimia nervosa
- Bariatric surgery
- Gastroenteritis
- Pneumonia
- Malaria
- Measles
- HIV/AIDS
- Hyperemesis
- Abnormal nutrient loss due to diarrhea or chronic small bowel illnesses (e.g., Crohn’s disease, untreated celiac disease)
- Poverty
- Homelessness
- Social isolation
Treatment
- Improve nutrition
- Supplementation
- Ready-to-use therapeutic foods
- Treat underlying cause
Management
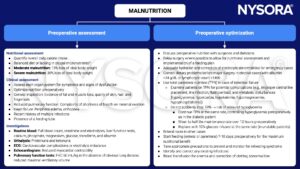
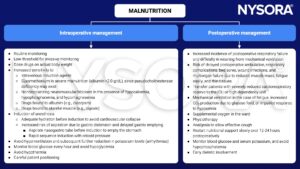
Keep in mind
- Malnutrition affects all systems, organs, and cells
- Treat all malnourished patients as if they have a full stomach (increased aspiration risk)
- Careful adjustment of drug dosing and understanding of the pharmacokinetics specific to the malnourished patient is vital
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 4 Gastrointestinal tract, Jackson MJ.
- Edwards S. Anaesthetising the malnourished patient. Update in Anaesthesia. 2016;31:31-37.
We would love to hear from you. If you should detect any errors, email us [email protected]