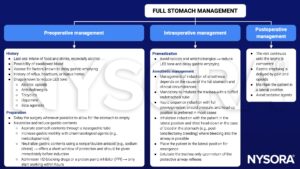
Learning objectives
- Outline the risks of having a full stomach in combination with anesthesia
- Describe the factors that delay gastric emptying
- Anesthetic management of a patient with a full stomach
Definition and mechanisms
- In anesthesia, the term “full stomach” applies to patients that have recently ingested foods and/or have pharmacologic, metabolic, anatomic, or hormonal conditions, which impair gastric emptying
- A full stomach and any reduction in the functional integrity of the lower esophageal sphincter (LES) predispose a patient to regurgitation
- The active process of vomiting and the passive process of regurgitation of gastric contents are more hazardous in a patient with a full stomach
- No patient can ever be assumed to have a completely empty stomach
General anesthesia suppresses the upper airway reflexes that prevent pulmonary aspiration of active or passively regurgitated gastric contents
- Aspiration of solid material can cause a mechanical obstruction with subsequent lung collapse, pneumonia, or abscess formation
- Aspiration of liquid (>25 mL, pH <2.5) can cause bronchospasm, pneumonitis, bronchopneumonia, and acute respiratory distress syndrome
Strategies to reduce the risk of pulmonary aspiration
- Minimize residual gastric volumes → fasting (stomach is considered “empty” within 6 hours after food and milky drinks, 4 hours after breast milk, and 2 hours after water)
- Rapidly secure the anesthetized airway
Emergency patients are more likely to have a full stomach as
- Presenting pathology causes a mechanical obstruction (e.g., laparotomy for small bowel obstruction)
- Surgery is urgent and cannot wait for the full fasting time
- The surgical pathology results in pain and anxiety
Risk factors
Factors delaying gastric emptying
- Mechanical obstruction of the gastrointestinal tract
- Ileus
- Following surgical manipulation of the bowel (postoperative)
- Recent trauma
- Electrolyte imbalance
- Peritonitis
- Pain
- Fear and anxiety
- Third trimester of pregnancy
- Drugs
Management
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 4 Gastrointestinal tract, Jackson MJ.
We would love to hear from you. If you should detect any errors, email us [email protected]