Learning objectives
- Describe the pathophysiology and possible complications of epiglottitis
- Diagnose epiglottitis
- Manage patients with (suspected) epiglottitis
Background
- Epiglottitis is a life-threatening inflammatory condition that causes swelling of the upper airways which can lead to asphyxia and respiratory arrest
- Usually caused by infection
- Noninfectious causes: Trauma from foreign objects, inhalation, and chemical burns
- Affects the epiglottis and nearby structures (arytenoids, aryepiglottic folds, vallecula)
- Symptoms can be exacerbated by patient discomfort or agitation
Pathophysiology
- The airway in the pediatric population differs from adults
- The epiglottis is located more superiorly and anteriorly
- More oblique angle with the trachea
- The narrowest part of the pediatric airway is the subglottis, in contrast to the glottis in adults
- The infant epiglottis is comprised of cartilage and far more pliant
- Infectious processes that lead to edema and mass increase of the epiglottis are more likely to cause symptoms in children
- Each inspiration pulls the edematous epiglottis over the laryngeal airway, causing symptoms
Complications
- Cellulitis
- Cervical adenitis
- Death
- Empyema
- Epiglottic abscess
- Hypoxia
- Meningitis
- Pneumonia
- Pneumothorax
- Prolonged ventilation
- Pulmonary edema
- Respiratory failure
- Sepsis
- Septic arthritis
- Septic shock
- Tracheostomy
- Vocal cord granuloma
- Ludwig angina-type submental infection
Signs & symptoms
- Sudden onset
- Fever
- (Severe) sore throat
- Difficulty swallowing
- Hypersalivation
- Stridor
- “Tripod position”
- Inability to lie flat
- Voice changes
- Dysphagia
- Anxiety
- Tachypnea
- Cyanosis
Diagnosis
- Oropharyngeal exam may lead to loss of airway
- Lateral neck radiograph: Swelling of the epiglottis (only perform in stable, cooperative patients)
- When epiglottitis is suspected, transfer the patient to the operating room for airway assessment
- Differential diagnosis: laryngotracheobronchitis (croup), airway obstruction from a foreign object, acute angioedema, caustic ingestion, diphtheria, peritonsillar/retropharyngeal abscess
Management
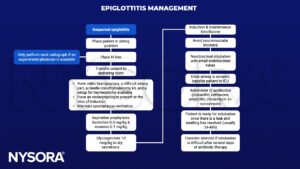
Keep in mind
- Do not agitate the patient
- Be prepared for sudden worsening of the clinical condition
- Oral exams may lead to loss of airway
Suggested reading
- Guerra AM, Waseem M. Epiglottitis. [Updated 2022 Oct 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430960/
- Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED. Epiglottitis: It Hasn’t Gone Away. Anesthesiology. 2016;124(6):1404-7.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com