Learning objectives
- Describe the physiological effects and possible complications of prone positioning
- Manage patients presenting for surgery in the prone position
Background
- Prone positioning is commonly used for access to the posterior head, neck, and spine during spinal surgery, access to the retroperitoneum and upper urinary tracts, and access to posterior structures when required during plastic surgery
- Prone surgery is associated with a variety of complications and requires specific considerations
Physiology
| Respiratory | Increased functional residual capacity |
| Increased arterial oxygen pressure | |
| Chest wall and lung compliance remain unchanged | |
| Cardiovascular | Reduced stroke volume |
| Compensatory sympathetic tachycardia and increase in peripheral vascular resistance | |
| Increased pulse pressure and stroke volume variation | |
| Cerebral blood flow | Reduced cerebral blood flow |
| Increased intracranial pressure | |
| Vessel distension | |
| Renal function | Slight increase in urine output |
Complications
- Pressure injuries
| Direct pressure injuries | Skin necrosis |
| Contact dermatitis | |
| Tracheal compression | |
| Salivary gland swelling | |
| Breast injury | |
| Injury to the genitalia | |
| Compression of the pinna | |
| Compression of the femoral neurovascular bundle | |
| Indirect pressure injuries | Macroglossia and orpharyngeal swelling |
| Mediastinal compression | |
| Visceral ischemia (liver, pancreas) | |
| Avascular necrosis of femoral head | |
| Peripheral vessel occlusion | |
| Limb compartment syndrome and rhabdomyolysis |
- Ophthalmic complications ranging from corneal abrasions to postoperative visual loss
- Direct pressure on the eye: central retinal artery occlusion
- No direct pressure on the eye: Ischemic optic neuropathy
- Risk factors: Atherosclerosis, diabetes, hypertension, male gender, blood loss, long duration of the procedure
- Prevention: Avoid direct ocular pressure
- Peripheral nerve injuries
- All superficial peripheral nerves should be considered at risk
- Usually does not present in the recovery room, 90% present within 7 days
- Can be sensory or mixed motor/sensory
- Risk factors: Male gender, prolonged hospital stay, diabetes, advanced age, extremes in BMI
- Prevention: Place arms at side, <90° at elbow or shoulder if arms are abducted, avoid direct pressure in the axilla, pad the elbows
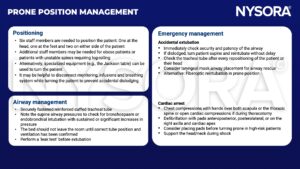
Management
Suggested reading
- Kwee MM, Ho YH, Rozen WM. The prone position during surgery and its complications: a systematic review and evidence-based guidelines. Int Surg. 2015;100(2):292-303.
- Feix B, Sturgess J. Anaesthesia in the prone position. Continuing Education in Anaesthesia Critical Care & Pain. 2014;14(6):291-7.
- Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. BJA: British Journal of Anaesthesia. 2008;100(2):165-83.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com