Learning objectives
- Manage patients with chronic obstructive pulmonary disease (COPD) in the pre-, and perioperative period
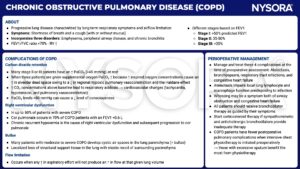
Definition
- COPD is an inflammatory lung disease characterized by abnormalities of the airways (bronchitis, bronchiolitis) and alveoli (emphysema), causing chronic dyspnea, cough, excessive sputum production, and progressive airway obstruction
Background information
- In 2017, 300 million people worldwide were living with COPD
Risk factors
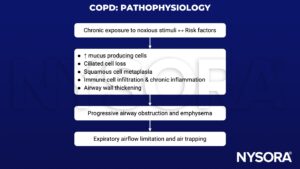
COPD is caused by a complicated interaction between chronic exposure to noxious stimuli, individual risk factors, and socioeconomic risk factors
Noxious stimuli
- Tobacco smoke
- Air pollution caused by burning carbon-based fuels or biomass
- Occupational exposure such as chemical fumes or other fine particulate matter
Individual risk factors
- History of previous lung infections, including tuberculosis
- Genetics
- Maternal and prenatal exposure
- Asthma
- Premature birth
Socio-economic risk factors
- Access to healthcare
- Diet
Pathophysiology
Exacerbation treatment
1. Assess severity
Use ABCDE approach – take arterial blood gas, perform chest X-ray, apply full ASA-monitoring
2. Treat symptoms
- Give supplemental O2 – titrate to achieve SaO2 of 88-92%
- Bronchodilators
- ↑ dose and/or frequency of short-acting bronchodilators
- Combine short-acting beta-2-agonists and anticholinergics
- Give long-acting beta-2-agonists when stable
- Give corticosteroids
- Give antibiotics if signs of bacterial infection
- If necessary, start noninvasive ventilation (NIV)
3. Identify and treat associated conditions
e.g., Heart failure, pulmonary embolism, arrhythmia
Anesthetic implications
Preoperative assessment
- Assess maximal level of exertion attainable
- Perform
- Routine preoperative blood tests
- Electrocardiogram – to exclude concomitant heart disease
- Chest X-ray – if evidence of current infection or recent worsening of symptoms
- Spirometry – to confirm the diagnosis and to assess the severity of COPD
- Treat symptoms aggressively
- If signs of active respiratory infection, postpone non-emergency surgery
- Strict smoking cessation
- Preoperative physiotherapy may help reduce the incidence of intraoperative bronchial plugging or pneumonitis
- Optimize nutritional status
- Obesity and underweight both increase perioperative risk
- Serum albumin level <35 mg/L is a strong predictor of postoperative pulmonary complications, give preoperative nutritional supplementation
Anesthetic regimen
- Regional anesthesia (RA) decreases postoperative pulmonary complications
- Light sedation, flexible positioning, or NIV might comfort patients who find it uncomfortable lying supine
- General anesthesia in COPD carries higher risk for laryngospasm, bronchospasm, cardiovascular instability, barotraumas, and hypoxemia
- To reduce the harmful effects of air trapping when mechanically ventilating
- Reduce the respiratory rate or the I:E ratio (to 1:3–1:5) to lengthen expiration
- Give PEEP to help keep small airways open during late exhalation
- Promptly treat bronchospasm
- Fully reverse the neuromuscular blocking agent before extubation
- Consider peri-extubation bronchodilator treatment
- NIV post-extubation reduces the work of breathing and air trapping and has been shown to reduce the need for reintubation in the postoperative period after major surgery
Suggested reading
- Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022;399(10342):2227-2242.
- National Institute for Health and Care Excellence. (2018) Chronic Obstructive Pulmonary Disease in over 16s: diagnosis and management (NICE guideline 115) available at https://www.nice.org.uk/guidance/ng115.
- Lumb AB, Biercamp C. Chronic obstructive pulmonary disease and anaesthesia. Continuing Education in Anaesthesia, Critical Care & Pain. 2014;14:1-5.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com