Learning objectives
- Description of restrictive lung disease
- Management of restrictive lung disease
Definition and mechanisms
- Diseases that restrict lung expansion, resulting in a decreased lung volume and total lung capacity, an increased work of breathing, and inadequate ventilation and/or oxygenation
- Often due to a decrease in the elasticity of the lungs themselves or caused by a problem related to the expansion of the chest wall during inhalation
- The normal lung tissue can be gradually replaced with scar tissue that is interspersed with pockets of air
- Characterized by a decrease in the forced vital capacity (FVC) and forced expiratory volume in one second (FEV1), however, the decline in FVC is more than that of FEV1, resulting in a higher than 80% FEV1/FVC ratio
- May be caused by the destruction of distal lung parenchyma due to infiltrates from inflammation, toxins (intrinsic conditions) as well as extra parenchymal conditions (extrinsic causes)
- Examples of restrictive lung diseases are asbestosis, sarcoidosis, and pulmonary fibrosis
Signs and symptoms
- Progressive exertional dyspnea
- Cough
- Shortness of breath
- Wheezing
- Chest pain
- Respiratory failure
Causes
| Intrinsic casuses | Extrinsic causes |
|---|---|
| Pneumoconiosis: for example asbestosis Radiation fibrosis Medication: amiodarone, bleomycin and methotrexate As a consequence of rheumatoid arthritis Hypersensitivity pneumonitis Acute Respiratory Distress Syndrome Infant respiratory distress syndrome Tuberculosis Idiopathic pulmonary fibrosis Idiopathic interstitial pneumonia Sarcoidosis Eosinophilic pneumonia Lymphangioleiomyomatosis Pulmonary Langerhans' cell histiocytosis Pulmonary alveolar proteinosis | Nonmuscular diseases: kyphosis, pectus carinatum, pectus excavatum Diseases restricting lower thoracic/abdominal volume, e.g. obesity, diaphragmatic hernia, or the presence of ascites Pleural thickening |
Complications
- Hypoxemia
- Muscle wasting and weight loss
- Chronic respiratory failure
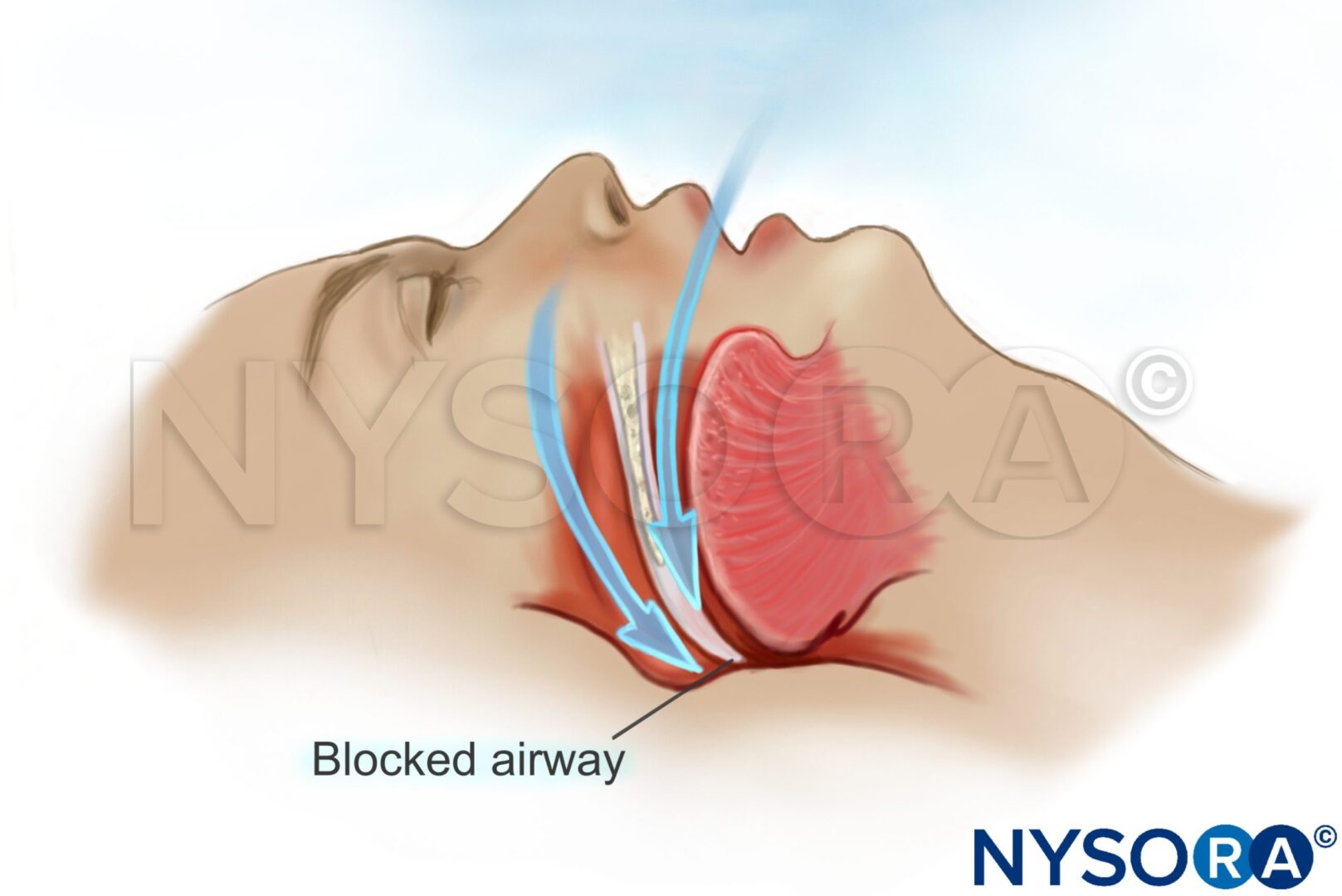
- Obstructive sleep apnea
- Pulmonary hypertension
- Cor-pulmunale
Diagnosis
- Pulmonary function tests
- Chest X-ray
- CT
- Bronchoscopy
- Pulse oximetry
- Arterial blood gas
Treatment
- Maximize pulmonary function with oxygen therapy, bronchodilators inhaled beta-adrenergic agonists and diuretics
- Management varies depending on the etiology of the restriction:
- Manage comorbid conditions
- Idiopathic pulmonary fibrosis: immunosuppression or anti-fibrotic agents such as pirfenidone and nintedanib
- Autoimmune conditions that lead to interstitial lung disease: immunosuppressants agents including steroids, mycophenolate mofetil, and cyclophosphamide
- Obesity: diet and physical exercise to lose weight
- Acute exacerbations are treated with steroids
Management
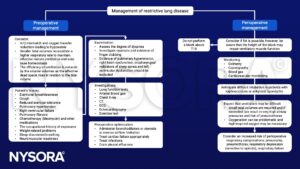
Postoperative management
- Consider sputum retention and basal atelectasis
- Extubate when compliant and awake so that coughing, mobilization, and physiotherapy are possible early
- Administer adequate analgesia
- Be aware of hypoxia and insidious hypercapnia
- Noninvasive ventilation, either CPAP or bilevel, can be used to facilitate postoperative lung volume recruitment and relieve the work of breathing as necessary
Suggested reading
- Vyas, Varsha & Gehdoo, Raghbirsingh & Hazari, Shruti & Hirpara, Parthkumar & Kaur, Mankeerat & Vashwani, Jayshree. (2021). Anesthesia Management in a Case of Restrictive Lung Disease. Journal of Research & Innovation in Anesthesia. 6. 49-50. 10.5005/jp-journals-10049-0104.
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Mangera Z, Panesar G, Makker H. Practical approach to management of respiratory complications in neurological disorders. Int J Gen Med. 2012;5:255-263.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com