Learning objectives
- Definition, classification, and management of inhalation injury
Definition and mechanisms
- Refers to damage to the respiratory tract or lung tissue from heat, smoke, or chemical irritants carried into the airway during inspiration
- The term is often used synonymously with smoke inhalation injury
Classification and causes
| Cause | Effect | |
|---|---|---|
| Upper airway injury | Hot air Steam | Laryngeal obstruction Bronchospasm |
| Tracheobronchial injury | Chemicals in smoke Inhalation of noxious gases (eg, chlorine) or liquids (eg, acid) Direct airway fire (eg, intraoperative) Aspiration | Mucosal slough Infection Bronchiolar plugging Atelectasis href="https://www.nysora.com/anesthesia/bronchospasm/">Bronchospasm |
| Parenchymal injury | Irritant gases | Pneumonia Pulmonary edema Alveolar capillary defect |
| Systemic toxicity | CO poisoning Hydrogen cyanide |
Signs and symptoms
- Voice changes
- Hoarseness
- Stridor
- Cough
- Respiratory distress
- Decreased level of consciousness or confusion
- Agitation
- Clinical hypoxemia (SpO2 <94%)
- Dizziness
- Nausea
- Vomiting
Management
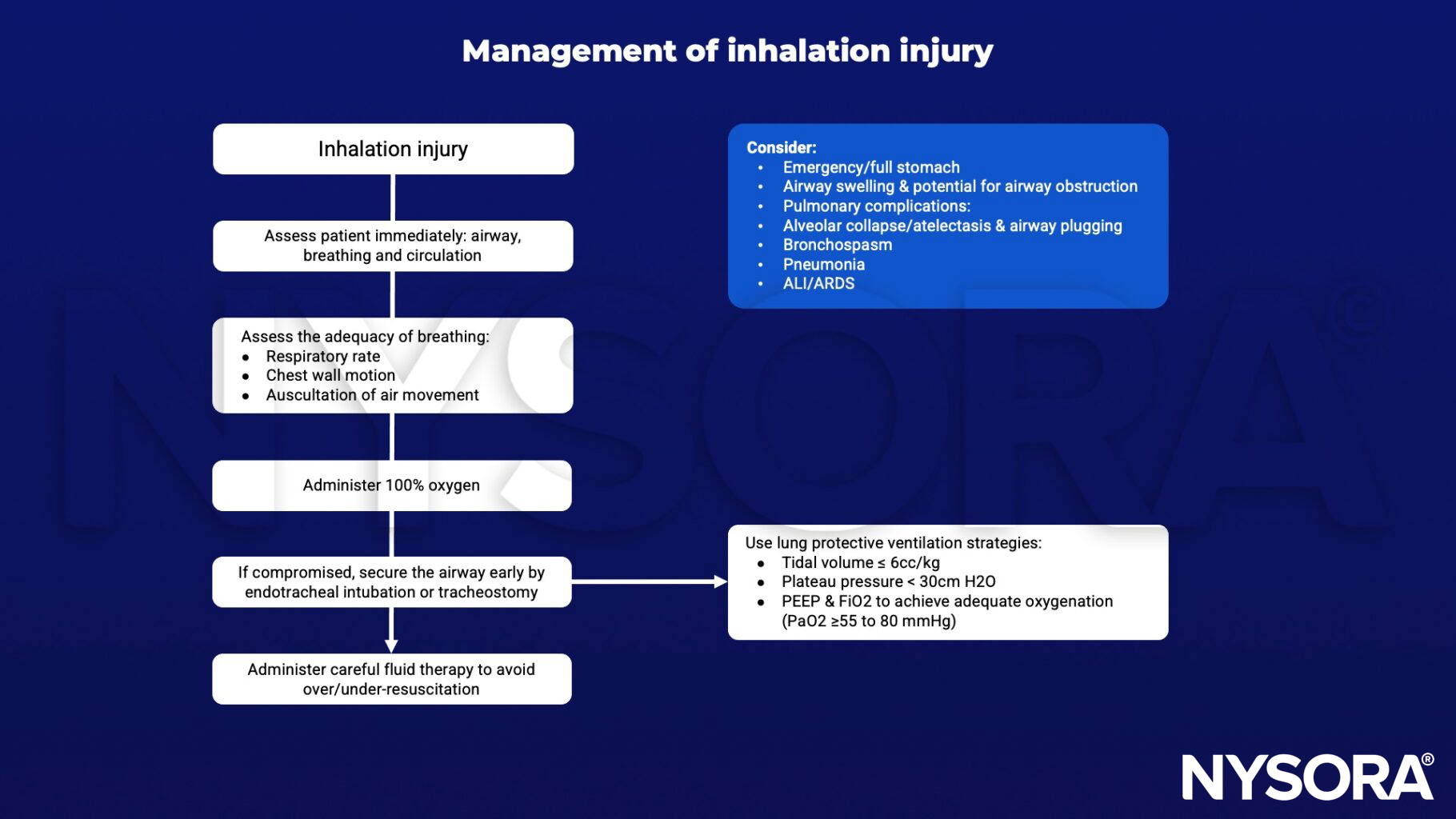
Keep in mind
General burn considerations:
- Hypovolemic shock
- Hypo or hyperthermia
- Rhabdomyolysis
- Cardiac depression
- DIC, consumptive coagulopathy
Suggested reading
- Preea Gill, FRCA, Rebecca V Martin, FRCA FFICM, Smoke inhalation injury, BJA Education, Volume 15, Issue 3, June 2015, Pages 143–148.
- Bittner EA, Shank E, Woodson L, Martyn JA. Acute and perioperative care of the burn-injured patient. Anesthesiology. 2015;122(2):448-464.
Clinical updates
Ding et al. (Frontiers in Immunology, 2025) demonstrate that bone marrow mesenchymal stem cells (BMSCs) alleviate smoke inhalation injury by promoting alveolar macrophage polarization from proinflammatory M1 to anti-inflammatory M2 via the CD200-CD200R pathway, with CD200 knockdown significantly reducing Arg-1/CD206 expression, increasing iNOS, and weakening M1/M2 ratio improvement both in vitro and in rat SII models. Mechanistically, BMSCs suppressed LPS/IFN-γ–induced JNK phosphorylation in macrophages, and CD200 silencing attenuated this inhibition, while in vivo CD200 knockdown diminished reductions in lung injury scores, BALF protein concentration, and proinflammatory cytokines (IL-1β, IL-6, TNF-α), confirming CD200 as a key immunomodulatory target for MSC-based therapy in early SII.
- Read more about the study HERE.
Milton-Jones et al. (Critical Care, 2023) report a RAND/UCLA-modified Delphi consensus identifying 74/140 statements as appropriate in burn inhalation injury (BII), supporting early fiberoptic bronchoscopy (FOB) for diagnosis and prognostication, initial intubation with ≥8.0 mm endotracheal tubes, lung-protective ventilation (tidal volume <6 mL/kg, plateau pressure <30 cmH₂O), and 5000 IU nebulized heparin (± salbutamol, N-acetylcysteine) for moderate–severe BII, while advising against non-protective ventilation, HFOV/HFPV, and prophylactic systemic antibiotics or corticosteroids. Key areas of uncertainty included the use of bronchoscopic grading to guide fluid resuscitation, the role of APRV in non-ARDS BII, and the efficacy of nebulized therapies in mild BII, highlighting the need for severity-stratified trials and improved bronchoscopic grading to better predict ARDS and mortality.
- Read more about the study HERE.