Learning objectives
- Identify the risk factors associated with extravasation injuries
- Recognize the differential diagnosis of extravasation injuries
- Manage and prevent extravasation injuries
- Recognize warning signs of extravasation injuries
Definition and mechanisms
- The unintentional injection or leakage of fluid in the perivascular or subcutaneous space
- Resulting from solution cytotoxicity, osmolality, vasoconstrictor properties, infusion pressure, and regional anatomical peculiarities
- May cause significant tissue necrosis resulting in the amputation of an extremity
Risk factors
- Preexisting cutaneous, vascular or lymphatic pathophysiology
- Fragile or mobile veins
- Site of injection
- Toxicity of the drug
- Amount of agent extravasated
- Duration of tissue exposure
- Decreased vigilance of doctor or patient
Three categories of anesthetic/ICU agents causing extravasation injury
| 1) Hyperosmolar agents | 2) Acids/alkalis | 3) Vascular regulators |
|---|---|---|
| Calcium chloride | Aminophylline | Epinephrine |
| Calcium gluconate | Amiodarone | Dobutamine |
| Glucose > 10% | Amphotericin | Dopamine |
| Magnesium sulphate 20% | Co-trimoxazole | Metaraminol |
| Mannitol 10% and 20% | Diazepam | Norepinephrine |
| Parenteral nutrition | Erythromycin | Prostaglandin |
| Potassium chloride | Phenytoin | Vasopressin |
| Sodium bicarbonate | Thiopental | |
| Sodium chloride > 0.9% | Vancomycin | |
| X-ray contrast media |
Differential diagnosis
- Propofol, ondansetron, rocuronium, and cyclizine can all cause discomfort or pain on injection
- Venous spasms may occur and can lead to localized skin blanching
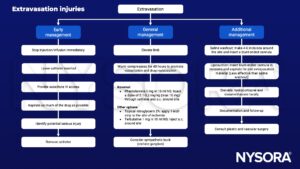
Management
Prevention
- Avoid IVs in the hand/wrist as the most appropriate site is considered to be the forearm
- Careful insertion of peripheral venous catheters
- Flush catheter with sterile saline
- Apply a suitable dressing to prevent movement of the catheter and avoid unreassuring IVs
- Inspect the catheterization site regularly
- Regulated delivery of intravenous fluids from continuous infusion pumps
- Hyperosmolar fluids, acidic or alkaline solutions, or infusates with irritant or vesicant properties should be given through central venous lines, if possible, or should be diluted or neutralized
- For slow infusion of high-risk drugs, a central line or peripherally inserted central catheter (PICC) line should be used
- Keep antidotes and the worksheet in the room with the patient
- 10 mg of phentolamine mesylate can be added to each liter of solution containing norepinephrine (the vasopressor effect of norepinephrine is not affected)
Suggested reading
- Al-Benna S, O’Boyle C, Holley J. Extravasation injuries in adults. ISRN Dermatol. 2013 May 8;2013:856541.
- Lake C, Beecroft CL. Extravasation injuries and accidental intra-arterial injection, Continuing Education in Anaesthesia Critical Care & Pain, Volume 10, Issue 4, August 2010, Pages 109–113.
- Schummer W, Schummer C, Bayer O, Müller A, Bredle D, Karzai W. Extravasation Injury in the Perioperative Setting. Anesthesia & Analgesia: March 2005 – Volume 100 – Issue 3 – p 722-727.
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com