Learning objectives
- Describe mucopolysaccharidoses
- Understand the anesthetic risk factors and complications associated with mucopolysaccharidoses
- Anesthetic management of a patient with mucopolysaccharidosis
Definition and mechanisms
- Mucopolysaccharidoses (MPS) are rare, inherited, lysosomal storage diseases characterized by deficiencies in different lysosomal enzymes involved in the metabolism of glycosaminoglycans (mucopolysaccharides)
- MPS causes an accumulation of glycosaminoglycans (mucopolysaccharides) in the brain, heart, liver, bone, cornea, and tracheobronchial tree
- Glycosaminoglycan accumulation in the upper airway results in hypertrophy of adenoids, tonsils, tongue (macroglossia), and laryngopharynx
- There are seven types and several subtypes of MPS, each with various clinical presentations → four broad categories
- MPS I, II, and VII affect soft tissue storage and the skeleton with or without brain disease
- MPS VI affects both soft tissues and the skeleton
- MPS IVA and IVA are primarily associated with skeletal disorders
- MPS III A-D are primarily associated with central nervous system disorders
- Autosomal recessive inheritance, except for MPS II, which is an inherited X-linked recessive disorder
- Patients with MPS often have a significantly shortened lifespan
| MPS type | Accumulated product | Enzyme | Gene/locus | Clinical manifestations |
|---|---|---|---|---|
| MPS I H | Heparan sulfate, dermatan sulfate | α-L-iduronidase | IDUA/4p16.3 | Intellectual disability, facial dysmorphism, dwarfism, cardiomegaly, valvular disease, OSA, and hepatosplenomegaly |
| MPS I S | ||||
| MPS I HS | ||||
| MPS II | Heparan sulfate, dermatan sulfate | Iduronate-2-sulfatase | IDS/Xq28 | Macroglossia, vocal cord enlargement, hydrocephalus, narrow airway, spinal stenosis, cardiomegaly, valvular disease, OSA, and hepatosplenomegaly |
| MPS III A | Heparan sulfate | Heparan N-sulfatase | SGSH/17q25.3 | Dementia, seizures, language skills, deafness, blindness, enlarged tonsils, adenoids, and respiratory infections |
| MPS III B | N-acetylglucosaminidase | NAGLU/17q21.2 | ||
| MPS III C | Heparan-α-glucosaminide N-acetyltransferase | HGSNAT/8p11.21 | ||
| MPS III D | N-acetylglucosamine 6-sulfatase | GNS/12q14.3 | ||
| MPS IV A | Keratan sulfate, chondroitin-6-sulfate | Galactose-6-sulfate sulfatase | GALNS/16q24.3 | Short stature, atlantoaxial instability, odontoid hypoplasia, pectus carinatum, spine deformities, hepatomegaly, and restrictive lung disease |
| MPS IV B | Keratan sulfate | β-galactosidase | GLB1/3p22.3 | |
| MPS VI | Dermatan sulfate | N-acetylgalactosamine-4-sulfatase | ARSB/5q14.1 | Short trunk, crouched stance, restricted joint movements, and heart disease |
| MPS VII | Heparan sulfate, dermatan sulfate, chondroitin-4,6-sulfate | β-glucuronidase | GUSB/7q11.21 | Skeletal dysplasia, short stature, nerve entrapment, developmental delay, and hepatomegaly |
Signs and symptoms, complications
- Damage to neurons
- Pain and impaired motor function resulting from compressed nerves or nerve roots in the spinal cord or peripheral nervous system
- Coarse facial features (flat nasal bridge, thick lips, and enlarged mouth and tongue)
- Short stature with disproportionately short trunk/torso (dwarfism)
- Abnormal bone size and/or shape (dysplasia) and other skeletal abnormalities
- Thickened skin
- Hepatosplenomegaly
- Hernias
- Carpal tunnel syndrome restricting hand mobility and function
- Recurring respiratory infections, obstructive airway disease, and obstructive sleep apnea (OSA)
- Heart disease, often involving enlarged or diseased heart valves
- Hyperactivity
- Depression
- Speech difficulties
- Hearing impairment
- Hydrocephalus
- Corneal clouding, degeneration of the retina, and glaucoma → vision problems
- Intellectual disabilities, developmental delays, or behavioral problems
Treatment
- Surgery to drain excess cerebrospinal fluid from the brain
- Surgery to free nerves and nerve roots compressed by skeletal and other abnormalities
- Surgery to correct hernias
- Corneal transplants to improve vision in patients with significant corneal clouding
- Surgery to remove the tonsils and adenoids to improve breathing in patients with obstructive airway disorders and OSA
- Enzyme replacement therapy (MPS I, II, IVA, VI, and VII) to reduce non-neurological symptoms and pain
Anesthesia challenges
Anesthetic risk factors
- Hypopharynx
-
- Hyperplasia of adenoids, tonsils, and pharyngeal tissue
- Narrow due to redundant tissue
- Neck pathology
- Cervical cord compression
- Short neck
- Atlantoaxial instability (only for MPS IV)
- Oral cavity
- Macroglossia (large tongue)
- Limited mouth opening
- Cardiac
- Coronary disease
- Valve disease
- Heart failure
- Significant arrhythmias
- Pulmonary hypertension
- Respiratory
- Restrictive lung disease
- Obstructive lung disease, OSA
- Breathing at closing capacity
- Recurrent pulmonary infections
- Pectus excavatum
- Kyphoscoliosis
- Narrow trachea
- Neurological
- Potential developmental delay, uncooperative
- Dural thickening can result in compressive myelopathy
- Hydrocephalus
- Other
-
- Hepatosplenomegaly
- Hepatic dysfunction
- Metabolic acidosis due to the inability to convert lactic acid to glycogen
- Hemorrhagic diathesis due to platelet dysfunction
Anesthetic complications that may occur during anesthesia in patients with MPS
- Inability to ventilate or intubate
- Temporary airway obstruction → can cause negative pressure (potentially obstructive) pulmonary edema
- Complete airway obstruction (mostly during induction or at extubation) → can cause hypoxemia and cardiac arrest
- Post-intubation problems
- Stridor
- Lower airway collapse/infection
- Need for reintubation or tracheostomy
Management
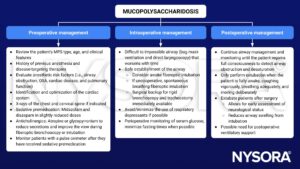
Keep in mind
- MPS are multisystem diseases, but the airway is the main concern (53% difficult intubation, 23% failed intubation)
- All MPS types, except for MPS III, have facial and airway characteristics which may challenge anesthetic airway management
Suggested reading
- Clark BM, Sprung J, Weingarten TN, Warner ME. Anesthesia for patients with mucopolysaccharidoses: Comprehensive review of the literature with emphasis on airway management. Bosn J Basic Med Sci. 2018;18(1):1-7.
- Walker R, Belani KG, Braunlin EA, et al. Anaesthesia and airway management in mucopolysaccharidosis. J Inherit Metab Dis. 2013;36(2):211-219.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com