Learning objectives
- Recognize the signs and symptoms of an upper respiratory tract infection
- Decide whether or not surgery should be postponed in children with an acute upper respiratory tract infection
- Anesthetic management of pediatric patients with upper respiratory tract infections
Definition and mechanisms
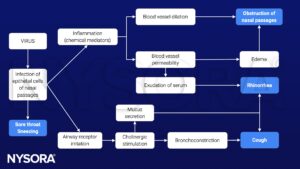
- An upper respiratory tract infection (URTI) is an illness caused by an acute infection, which involves the upper respiratory tract, including the nose, sinuses, pharynx, larynx, or trachea
- URTIs are characterized by cough, nasal congestion and discharge, sore throat, and sneezing
- URTIs include the common cold, epiglottitis, tonsillitis, rhinitis, pharyngitis, laryngitis, sinusitis, and otitis media
- Children experience 6 to 8 URTIs per year
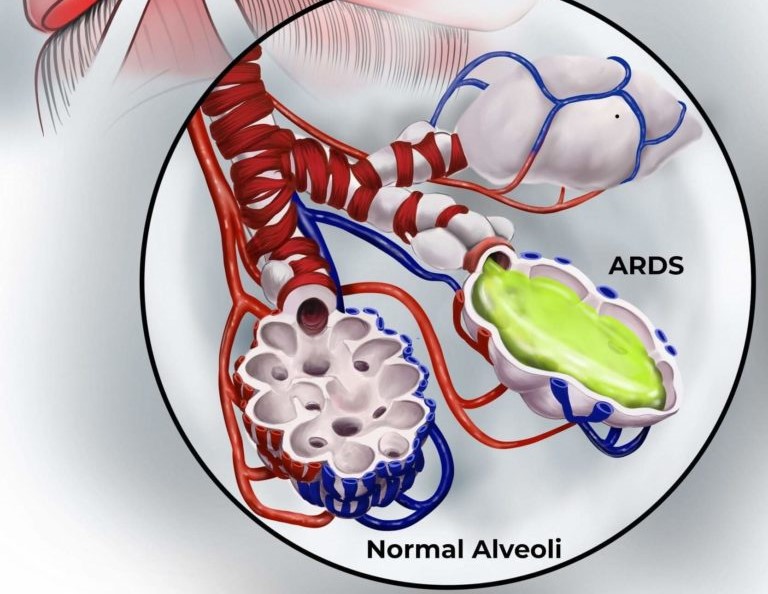
- Risk of perioperative adverse respiratory complications (i.e., coughing, breath holding, laryngospasm, bronchospasm, airway obstruction, oxygen desaturation <90%, atelectasis, post-extubation stridor, pneumonia, and unanticipated tracheal intubation or reintubation) is greatest during acute infection but remains increased for 2-6 weeks after URTI
- Independent risk factors for adverse respiratory events in children with active URTI include intubation, prematurity (<37 weeks), child <1 year, history of asthma or atopy, passive smoking, airway surgery, presence of copious secretions, nasal congestion, parental confirmation “my child has a cold”, snoring, and use of an endotracheal tube (ETT)
- Airway hyperreactivity is present for up to 6-8 weeks following a URTI
Signs and symptoms
- Cough
- Runny nose
- Nasal congestion
- Sore throat
- Headache
- Low-grade fever
- Facial pressure
- Sneezing
- Malaise
- Hoarse voice
- Fatigue and lack of energy
- Red eyes
- Swollen lymph nodes
Causes
- 95% of URTIs are secondary to viral causes, with rhinoviruses accounting for 30-40% of infections
Pathophysiology
Treatment
- Rest
- Fluids to stay hydrated
- Over-the-counter pain medications
- Antibiotics in case of bacterial origin (i.e., penicillin or amoxicillin)
Management

Preoperative assessment
- Parents statement
- Check for the presence of respiratory and cardiovascular comorbidities
- Monitor vital signs and baseline saturation
- Anticipate perioperative adverse respiratory events
- Chest X-ray if physical examination suggests signs of lower respiratory tract involvement
- Categorize URTI based on medical history and physical examination
- Mild URTIs: Clear runny nose, dry cough, appear healthy otherwise, clear lungs to auscultation, no fever
- Moderate URTIs: Green runny nose, mild moist cough, no wheezing or involvement of lower respiratory tract, no fever or irritability for 1-2 days
- Severe URTIs: Green runny nose, productive cough, mucopurulent secretion, nasal congestion, fever >38°C, severe sore or scratchy throat, pulmonary involvement (lower respiratory tract), wheezing, and lethargy
Anesthetic management
- Goal: Minimize secretions and avoid or limit stimulation of a potentially irritable airway
- Experienced pediatric anesthesia team
- Preoperative bronchodilators 10-30 min before surgery to reduce bronchoconstriction and perioperative respiratory events
- Humidifiers may help to clear secretions and prevent bronchial mucus plugging
- Combining β2-agonist (e.g., salbutamol) with inhaled corticosteroids is more effective in minimizing bronchoconstriction due to intubation compared to inhaled β2-agonist alone
- Avoid tracheal intubation, particularly in children <5 years
- A laryngeal mask airway or facemask is preferred
- IV lidocaine may be helpful in reducing the laryngospasm reflex
- Less adverse respiratory events with propofol than sevoflurane as induction agent
- Maintenance of anesthesia: Intravenous or inhalation techniques, anesthesia should be deep enough
- Suction airway only under deep anesthesia
Keep in mind
- Children with active and recent URTI are at increased risk of perioperative respiratory complications
- Assessment of suitability of any child with URTI symptoms for surgery includes the child’s age and presenting symptoms, frequency of URTIs, urgency and type of procedure, and presence of comorbidities
- The decision to postpone or proceed with surgery for children with URTI should be made on an individual basis by considering the presence of identified risk factors and the anesthesiologist’s experience
Suggested reading
- Lema GF, Berhe YW, Gebrezgi AH, Getu AA. Evidence-based perioperative management of a child with upper respiratory tract infections (URTIs) undergoing elective surgery; A systematic review. International Journal of Surgery Open. 2018;12:17-24.
- Regli A, Becke K, von Ungern-Sternberg BS. An update on the perioperative management of children with upper respiratory tract infections. Curr Opin Anaesthesiol. 2017;30(3):362-367.
- Tait AR, Malviya S. Anesthesia for the child with an upper respiratory tract infection: still a dilemma?. Anesth Analg. 2005;100(1):59-65.
We would love to hear from you. If you should detect any errors, email us [email protected]