Learning objectives
- Identify conditions requiring a tracheostomy
- Management of a tracheostomy
Definition and mechanism
- Surgical incision into the trachea that forms a temporary or permanent opening, when intubation is expected to last > 1-2 weeks
- Very short and wide tube directly place into trachea → decreased risk of pneumonia
- Commonly performed in the OR under general anesthesia
- Create access to remove secretions from the lungs
- Often needed when health problems require long-term use of a machine (ventilator) to help you breathe
- Emergency tracheostomy is performed when the airway is suddenly blocked due to a traumatic injury to the face or neck
- Patients with a tracheostomy can be weaned from a ventilator faster than patients with a ETT
- Consider: shared airway, difficult airway
- Close communication with surgeon, backup plan discussed
Indications
- Prolonged mechanical ventilation
- Pulmonary toilet
- Airway protection
- Part of a surgical procedure
- Upper airway obstruction
- Aspiration risk
Conditions requiring a tracheostomy
- Congenital abnormalities of the airway
- Airway burns from the inhalation of corrosive material
- Obstruction of the airway by a foreign object
- Obstructive sleep apnea
- Injury to the larynx
- Severe neck or mouth injuries
- Bilateral vocal cord paralysis
- Facial burns or surgery
- Chronic lung disease
- Anaphylaxis
- Coma
- Cancers that affect the head and neck
- Infection
- Neck tumors
- Paralysis of the muscles used in swallowing
- Injury to the chest wall
- Dysfunction affecting the diaphragm
Complications
| Early | Short-term | Long-term |
|---|---|---|
| Hemorrhage | Blockage | Tracheomalacia |
| Aspiration | Tube displacement | Tracheal stenosis |
| Pneumothorax | Pneumothorax | Tracheocutaneous fistula |
| Failure of procedure | Surgical emphysema | Decannulation problems |
| Infection | ||
| Delayed hemorrhage | ||
| Tracheal necrosis | ||
| Tracheo-arterial fistula |
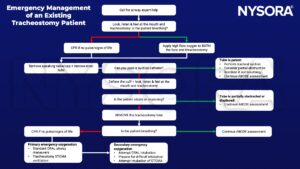
Management
- High-flow nasal oxygen therapy to slow the time to desaturation where intubation or face-mask ventilation is difficult/impossible
- Risk on fire as FiO2 is close to 1.0 if diathermy is used
- Check the position and size of the tracheostomy tube with a combination of capnography + endoscopy + cuff pressure
- The tube is too short: the cuff may herniate up into the superior larynx (within the vocal cords) thereby causing reduced pulmonary compliance, persistent cuff leaks, or tracheal damage
- Tube too long: risk of endobronchial tube placement
Keep in mind
- A laryngectomy tube can be used instead of a tracheostomy tube for intraoperative ventilation of the lungs during surgery
- Difficult BMV & supraglottic device ventilation (air leak)
- Dangerous placement of ETT (direct vision preferred)
- Comorbid disease:
- ICU patient with multi-organ failure, sepsis, lung injury, etc
- Neuromuscular disorders, chronic high spinal cord injury
- Ensure emergency tracheostomy equipment is available: various sizes of cuffed/uncuffed tracheostomy tubes, suction catheters, graspers, Ambu bags & ties
Suggested reading
- Rosero EB, Corbett J, Mau T, Joshi GP. Intraoperative Airway Management Considerations for Adult Patients Presenting With Tracheostomy: A Narrative Review. Anesth Analg. 2021;132(4):1003-1011.
- Lewith H, Athanassoglou V. Update on management of tracheostomy. BJA Educ. 2019;19(11):370-376.
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com