Learning objectives
- Definition of idiopathic thrombocytopenia purpura (ITP)
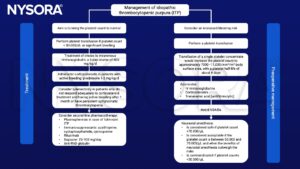
- Treatment and perioperative management of ITP
Definitions and mechanisms
- Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disease characterized by a low platelet count, purpura, and hemorrhagic episodes
- Resulting in easy or excessive bruising and bleeding due to unusually low levels of platelets
- The immune system produces antibodies against platelets
- Most often against platelet membrane glycoproteins IIB-IIIa or Ib-IX
- Normal platelet count is between 150.000 and 450.000, the platelet count is less than 10.000 with ITP
- Pregnant women with ITP have an increased incidence of fetal loss, a low fetal birth rate, and a higher incidence of premature births
- Two types:
- Acute thrombocytopenic purpura
- Affects young children between 2-6 years, often following a coral infection
- Starts suddenly and symptoms usually disappear in less than 6 months, often within a few weeks
- Most common form and resolves spontaneously
- Chronic thrombocytopenic purpura
- Onset can happen at any age
- Symptoms can last a minimum of 6 months to several years or a lifetime
- More common in adults and in females
- Requires continual follow-up care
- Acute thrombocytopenic purpura
Signs and symptoms
- Easy or excessive bruising
- Petechiae
- Bleeding from the gums or nose
- Blood in urine or stools
- Unusually heavy menstrual flow
Complications
- Subarachnoid or intracerebral hemorrhage
- Lower gastrointestinal bleeding
Causes
- Medication (the medication absorbs the platelet cell membrane)
- Infection: the virus that causes chickenpox, hepatitis C, and AIDS
- Pregnancy
- Immune disorders: rheumatoid arthritis, lupus
- Cancer: low-grade lymphomas and leukemia
- The cause is sometimes unknown
Diagnosis
- Complete blood count
- Low platelet count, usually <40×10^9/L for over three months
- Bleeding time
- Blood and urine tests to detect a possible infection
- Antiplatelet antibody test
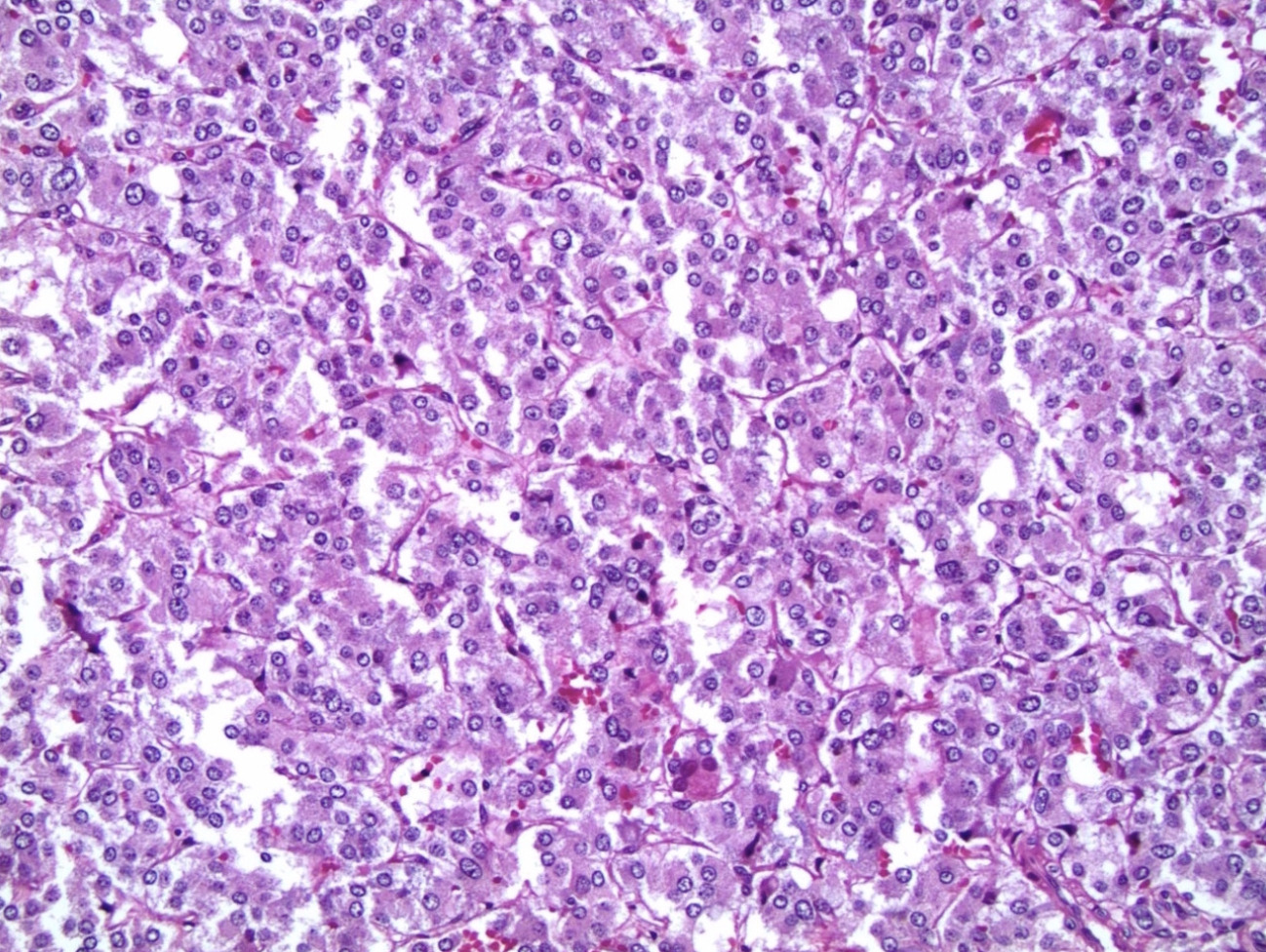
- Bone marrow examination shows an increased number of megakaryocytes
Management
Suggested reading
- Toyomasu Y, Shimabukuro R, Moriyama H, et al. Successful perioperative management of a patient with idiopathic thrombocytopenic purpura undergoing emergent appendectomy: Report of a case. Int J Surg Case Rep. 2013;4(10):898-900.
- Ramalingam, G., Jones, N., Besser, M., 2016. Platelets for anaesthetists—part 1: physiology and pathology. BJA Education 16, 134–139.
- Warrier R, Chauhan A. Management of immune thrombocytopenic purpura: an update. Ochsner J. 2012;12(3):221-227.
- Guidelines for the investigation and management of idiopathic thrombocytopenic purpura in adults, children and in pregnancy. 2003. British Journal of Haematology 120, 574–596.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com