Learning objectives
- Description and types of heparin-induced thrombocytopenia (HIT)
- Management of HIT
Definition and mechanisms
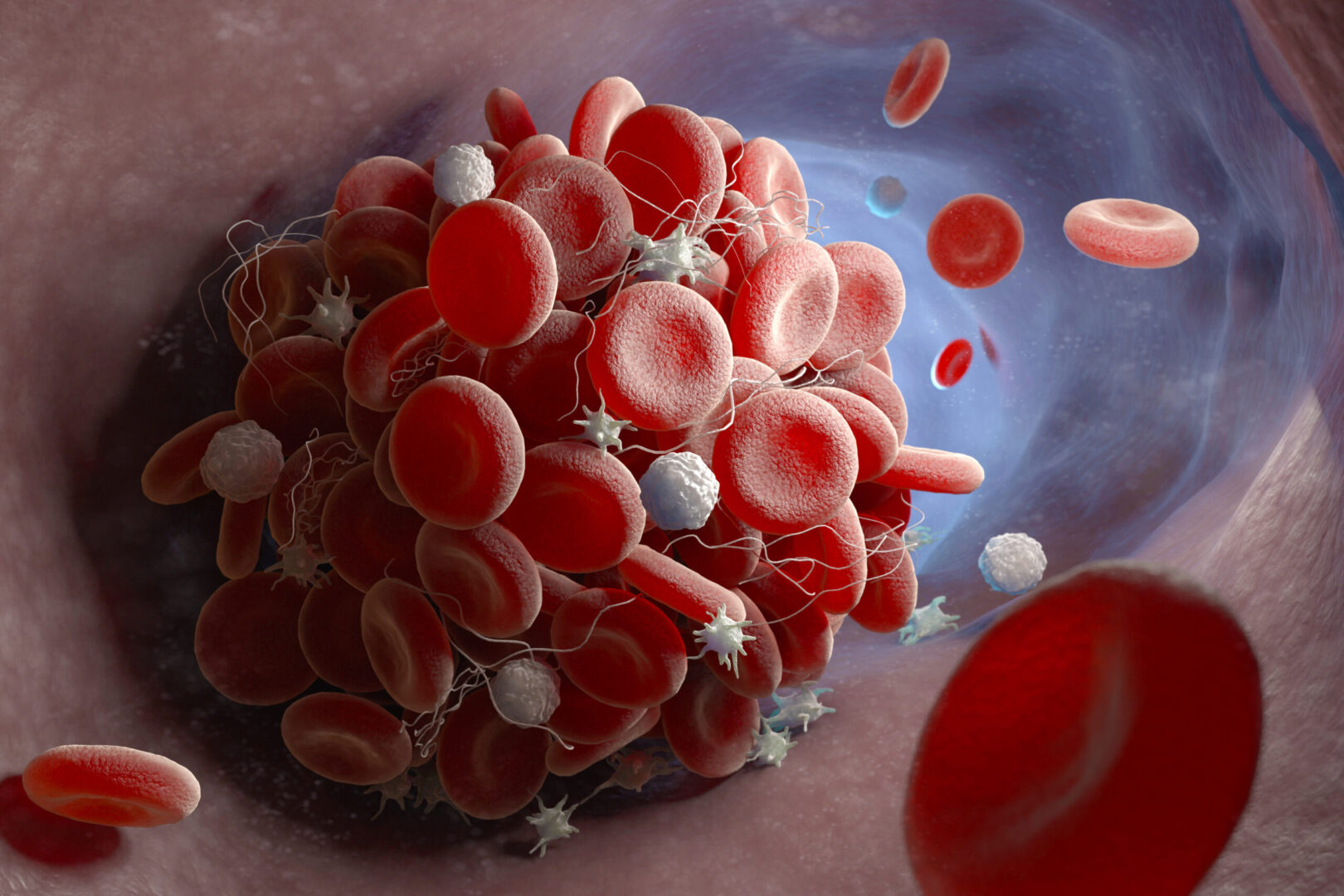
- Heparin-induced thrombocytopenia (HIT) is a potentially life-threatening complication of heparin therapy leading to the formation of new blood cloths rather than preventing new blood clots
- HIT occurs in approximately 5% of patients taking heparin for > 4 days and is more common in women
- Administration of heparin can lead to the formation of an immune complex between heparin and a specific blood factor (PF4) released by platelets
- This complex triggers the immune system to form antibodies that bind to the heparin-PF4 complex leading to the clotting of platelets
- The clotting platelets release more PF4, causing a chain reaction
- Immune-mediated HIT usually occurs between 5-14 days after first starting heparin therapy with typically a decrease of platelets by > 30%
- Platelets rarely drop <20
- Mortality is 10-20%
Two types of HIT
| HIT I (nonimmune) | HIT II (immune-mediated) |
|---|---|
| Occurs 1-4 days after initiation of therapy Mild thrombocytopenia despite continued use of heparin Usually resolves spontaneously Occurs primarily with high-dose intravenous heparin Usually no clinical sequelae Treatment is not required Occurs most frequently | Occurs 5-4 days after initial therapy Thrombocytopenia is usually severe Occurs with any dose of heparin by any route May cause serious thromboembolic complications Heparin must be discontinued Occurs less frequently, however, is dangerous |
Signs and symptoms
- Low levels of platelets may be a sign of HIT when taking heparin
- About 50% of patients with HIT develop deep vein thrombosis or pulmonary embolism and symptoms include:
- Pain, swelling, redness, or tenderness in the arm or leg
- Sudden sharp pain in the chest
- Hypertension
- Feeling faint, dizzy, or light-headed
- Tachycardia
- Coughing and wheezing
- Feeling out of breath
- Excessive sweating
- Fever and chills
Risk factors
- Gender
- Taking certain low-molecular-weight heparin (LMWH) instead of unfractionated heparin (UFH)
- Taking heparin after surgery
Complications
- New venous or arterial thrombotic event
- Treatment-related bleeding
- Limb amputation
- Venous gangrene
4Ts probability scale
This scale can be used to estimate the probability of a patient having HIT
- High: 6-8 points
- Intermediate: 4-5 points
- Low: 0-3 points
| Thrombocytopenia | Timing of onset of decrease in platelet count (or other sequelae of HIT) | Thrombosis or other sequelae | Other causes of decrease in platelet count |
|---|---|---|---|
| 2 points if >50% decrease in platelet count to a platelet count nadir of ≥20×109 /L | 2 points if onset is 5-10 days after starting heparin, or <1 day if there has been recent heparin use (within past 30 days) | 2 points if there is a proved new thrombosis, skin necrosis, or acute systemic reaction after intravenous unfractionated heparin bolus | 2 points if none evident |
| 1 point if 30-50% decrease in platelet count, or if the nadir is 10-19×109 /L | 1 point if onset is >10 days after starting heparin or if timing is unclear; or if <1 day after starting heparin with recent heparin use (past 31-100 days) | 1 point if there is progressive or recurrent thrombosis, erythematous skin lesions at injections sites, or suspected thrombosis (not proved) | 1 point if there is another possible cause |
| 0 points if <30% decrease in the platelet count, or if the nadir is <10×109 /L | 0 points if onset is within four days of first time heparin use (no recent heparin) | 0 points if there is no thrombosis or other finding | 0 points if there is another definite cause |
Diagnosis
- Normal platelet count before the commencement of heparin
- Thrombocytopenia is defined as a drop in platelet count by 30% < 100 x 109/l or a drop of > 50% from the patient’s baseline platelet count
- The onset of thrombocytopenia typically 5–10 days after initiation of heparin treatment, which can occur earlier with previous heparin exposure (within 100 days)
- Acute thrombotic event
- The exclusion of other causes of thrombocytopenia
- The resolution of thrombocytopenia after cessation of heparin
- IT antibody seroconversion
Prevention
- Avoid heparin where possible
- Use low molecular weight heparin instead of unfractionated heparin where possible
- Monitor platelet counts daily in high-risk patients
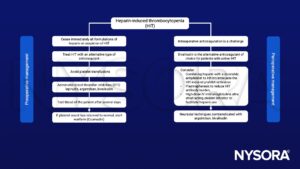
Management
Suggested reading
- Andreas Koster, Michael Nagler, Gabor Erdoes, Jerrold H. Levy; Heparin-induced Thrombocytopenia: Perioperative Diagnosis and Management. Anesthesiology 2022; 136:336–344
- Linkins LA. Heparin induced thrombocytopenia. BMJ. 2015;350:g7566. Published 2015 Jan 8.
- Ahmed I, Majeed A, Powell R. Heparin induced thrombocytopenia: diagnosis and management update. Postgrad Med J. 2007;83(983):575-582.
- Baroletti, S.A., Goldhaber, S.Z., 2006. Heparin-Induced Thrombocytopenia. Circulation 114, e355–e356.
We would love to hear from you. If you should detect any errors, email us [email protected]