Learning objectives
- Describe the etiology of hemolytic uremic syndrome
- Management of hemolytic uremic syndrome
Definition and mechanisms
- Hemolytic uremic syndrome (HUS) is a triad of renal failure, hemolytic anemia, and thrombocytopenia and is the most common cause of renal failure in infancy and childhood
- HUS can lead to widespread inflammation and thrombotic microangiopathy, the formation of platelet microthrombi in the walls of small blood vessels
- Most cases occur after infectious diarrhea due to a specific type of E. coli
- Other causes include S. pneumonia, Shigella, Salmonella, and certain medications
- Two predominant types:
- Typical HUS
- Preceded by 4-6 days of diarrhea
- Most commonly caused by infection with Shiga toxin-producing E. coli (O157:H7)
- The mortality rate is 3%-5%
- Approximately two-thirds of children require dialysis although 85% regain normal renal function
- Atypical HUS
- 60-50% can be attributed to dysregulation of the alternative complement pathway
- Involves mutations in factor H, factor I, CD46/MCP, factor B, and C3 components
- A mortality rate of up to 25% in the acute phase
- 50% of patients require renal replacement therapy at some point
- Typical HUS
- The first symptoms of infection can emerge between 1 to 10 days later, but usually after 3 to 4 days
- Affects about 1.5 per 100,000 people each year
- A multisystemic disease affecting:
| Cardiovascular system | Myocarditis Congestive heart failure Severe Hypertension |
| Respiratory system | Severe respiratory insufficiency Pulmonary edema Congestive heart failure |
| CNS | Drowsiness Seizures Hemiparesis Coma |
| Biochemical | Evidence of Acute kidney injury (AKI) Acid-base and electrolyte disturbances Abnormal liver function tests associated with hepatitis |
| Hematological | Hemolysis rapidly appears Hemoglobin falls to as low as 4 g/L Thrombocytopenia Hepatosplenomegaly |
| Renal system | Proteinuria, hematuria and oliguria leading to anuria |
| Gastrointestinal tract | Hemorrhagic gastritis |
| Immunological | Severe infections: peritonitis, meningitis, osteomyelitis |
Signs and symptoms
- Abdominal pain, cramping, or bloating
- Bloody diarrhea
- Fever
- Vomiting
- Pale coloring, including loss of pink color in cheeks and inside the lower eyelids
- Extreme fatigue
- Shortness of breath
- Easy bruising or unexplained bruises
- Unusual bleeding
- Decreased urination or blood in the urine
- Edema
- Confusion, seizures, or stroke
- High blood pressure
- Low platelets
Complications
- Kidney failure
- Hypertension
- Stroke or seizures
- Coma
- Clotting problems
- Heart problems
- Digestive tract problems
Diagnosis
- Travel and dietary history
- Complete blood count: anemia (Hb < 10 g/dl) and thrombocytopenia
- Comprehensive metabolic panel (elevated creatinine, elevated indirect bilirubin, and elevated lactate dehydrogenase)
- Urinalysis
- Peripheral smear
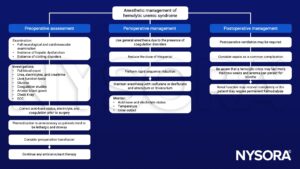
Treatment
- Fluid resuscitation
- Treat hyperkalemia
- Dialysis
- Control hypertension with standard antihypertensive agents
- Steroids
- Blood transfusion
- Plasmapheresis
Management
Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Noris M, Remuzzi G. Hemolytic uremic syndrome. J Am Soc Nephrol. 2005;16(4):1035-1050.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com