Learning objectives
- Getting familiar with an evidence-based, structured approach to managing a difficult airway
Signs and symptoms
- Failure to ventilate or intubate a patient
- Airway edema from repeated intubation attempts
- Desaturation and subsequent hypoxia
- Absent or minimal end-tidal CO2
- Insufficient tidal volumes
- Cyanosis
- Cardiac arrest
Complications contributing to difficult airway management
- History of difficult intubation
- Distorted airway anatomy
- Snoring
- Obstructive sleep apnea
- Diabetes mellitus
- Increasing Mallampati and modified Mallampati scores
- Thyromental distance < 6 cm
- Sternomental distance <12.5 cm
- Interincisor distance < 4 cm
- Large neck circumference
- Reduced neck mobility
- Acquired or congenital disease states:
- Ankylosing spondylitis
- Degenerative osteoarthritis
- Treacher–Collins
- Klippel–Feil syndrome
- Down syndrome
- Face-mask ventilation:
- Obesity
- Large tongue
- Beard
- Toothless mouth
- Distorted facial anatomy
Guidelines
Management
Keep in mind
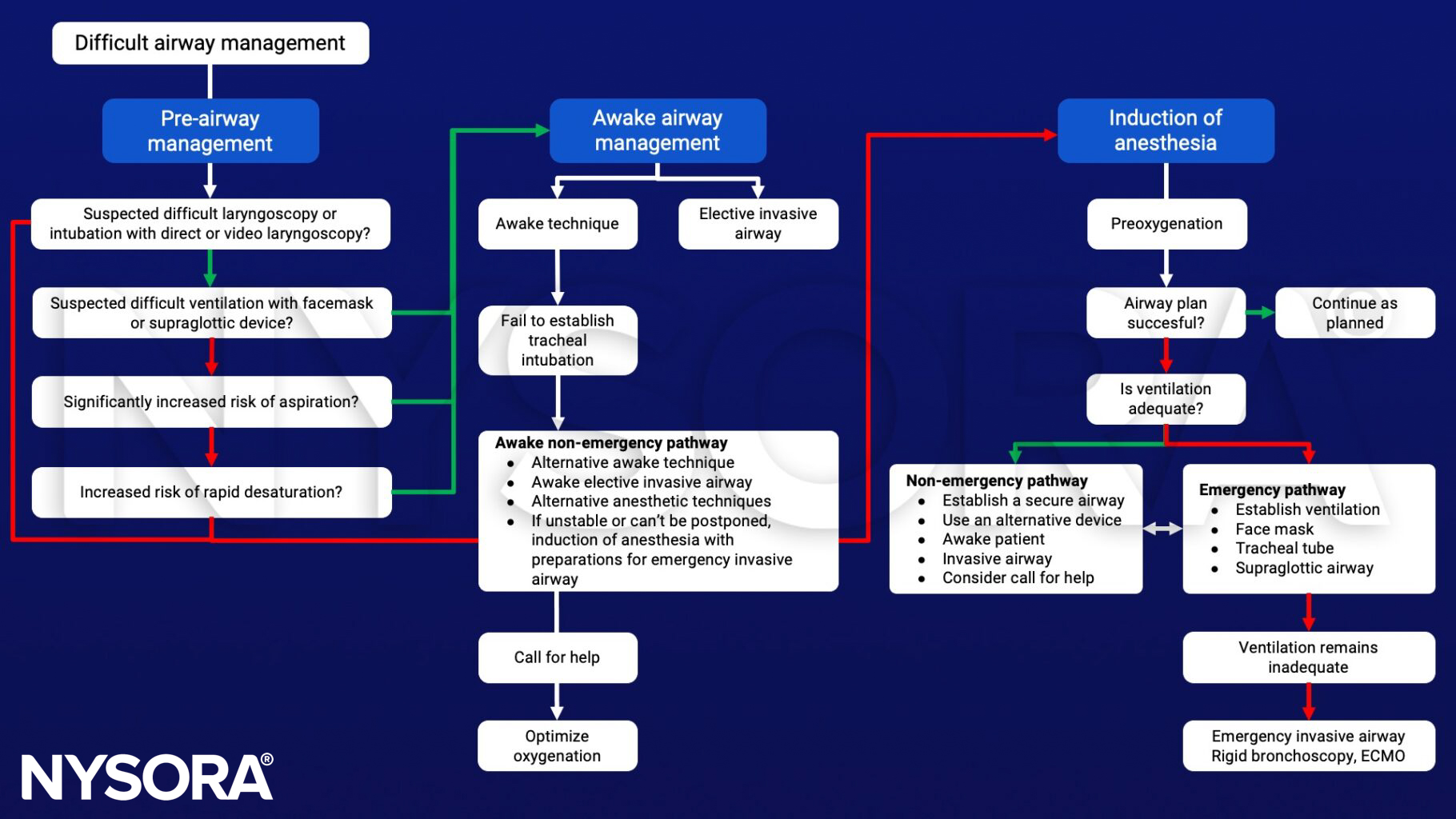
- Always screen and anticipate a suspected difficult airway
- Decide whether awake intubation is indicated
- Planning for a failed intubation should be part of every pre-induction briefing
- Ensure proper positioning of the patient
- Preoxygenation is recommended for all patients, apnea time without desaturation (SaO2 <90%) is generally limited to 1-2 minutes, and with proper preoxygenation, this period can be extended to 8 minutes
- All anesthesiologists should be trained to use, and have immediate access to a video laryngoscope
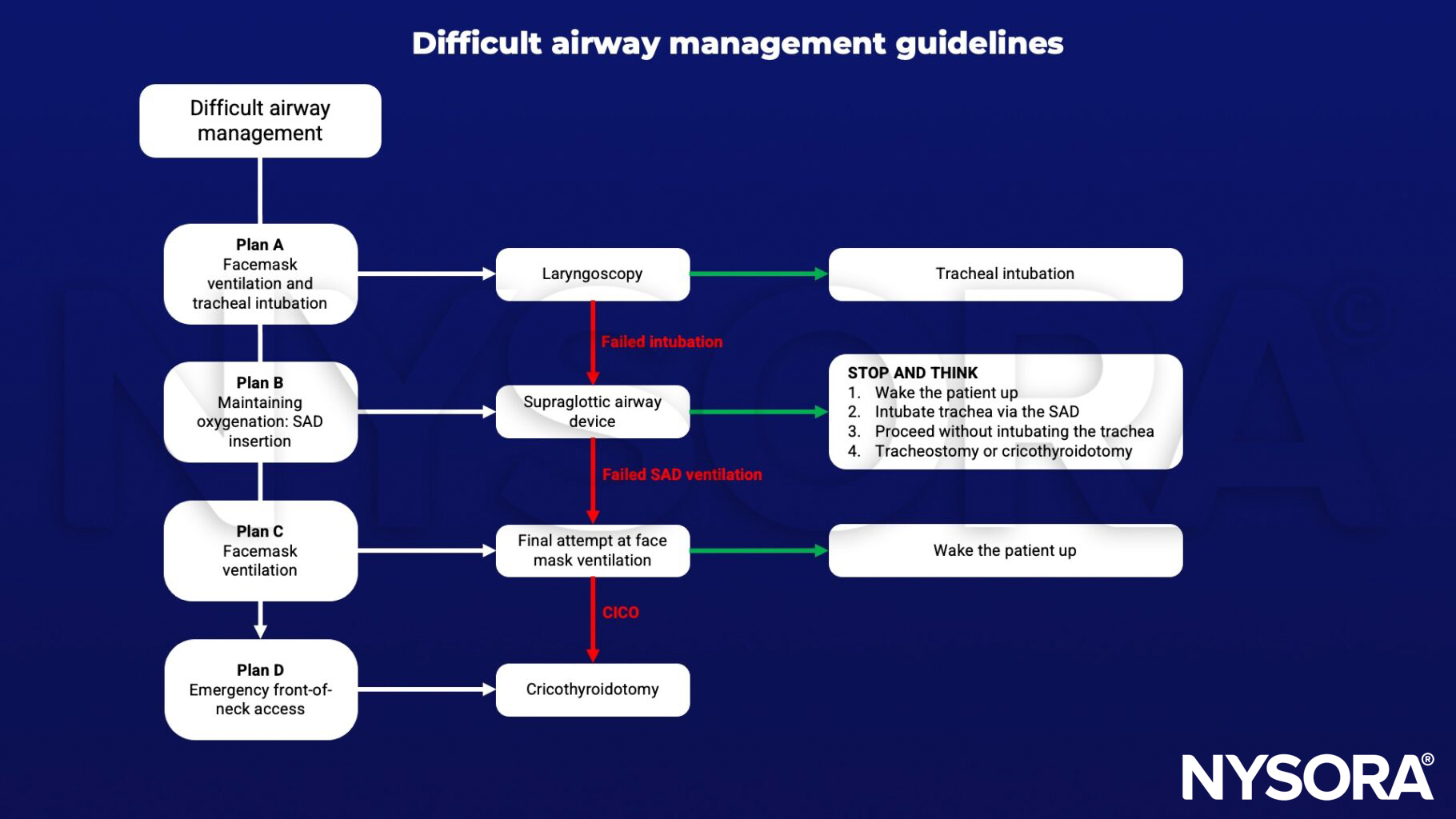
- In case of a failed intubation, a supraglottic airway is recommended to maintain adequate oxygenation
- In case of a failed intubation or ventilation, consider calling for help early
- If both endotracheal intubation and ventilation with an SGA fail after having ensured adequate depth of anesthesia and relaxation, the safest option is to attempt mask ventilation and when successful, wake the patient up and postpone surgery
- In a CICO (can’t intubate can’t oxygenate) situation, scalpel cricothyroidotomy is recommended as the preferred rescue technique
Suggested reading
- Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136(1):31-81.
- Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827-848.
Clinical updates
Ahmad et al. (British Journal of Anaesthesia, 2025) present the updated Difficult Airway Society (DAS) guidelines for unanticipated difficult tracheal intubation in adults, based on a systematic review of 1,241 papers and a Delphi consensus process. The 2025 update maintains the Plan A→B→C→D algorithm but shifts emphasis toward maximizing first-pass success, continuous oxygenation, early use of videolaryngoscopy, and rapid progression between plans. The guideline also strengthens recommendations on human factors, team communication, physiologically difficult airways, and mandatory capnography confirmation, reinforcing a systems-based approach to improving outcomes in high-risk airway scenarios.
Markham et al. (Anesthesia & Analgesia, 2025) conducted a prospective, randomized, crossover trial in 147 adults with potentially difficult airways and demonstrated that trans-tube-in-pharynx (TTIP) ventilation achieved a 93.4% success rate, compared with 84.6% for facemask ventilation, using visible ETCO₂ within three breaths as the primary endpoint. Notably, TTIP successfully rescued 100% of failed mask ventilation cases, with only 0.7% failing both techniques. These findings suggest TTIP may represent a simple, equipment-light rescue option in difficult airway and potential CICO scenarios, warranting consideration in airway management algorithms.
Kristensen et al. (Current Opinion in Anesthesiology, 2025) review contemporary tracheal intubation strategies in head and neck surgery, emphasizing awake tracheal intubation as the gold standard in anticipated difficult airways due to tumor burden, prior radiation, or airway distortion. The authors highlight routine use of videolaryngoscopy, flexible bronchoscopy, structured preoperative imaging, and explicit rescue planning, including front-of-neck access. These updates reinforce a patient-specific, preparation-focused approach to difficult airway management, with strong emphasis on maintaining spontaneous ventilation when airway compromise is suspected.
- Read more about this study HERE.
Kojima et al. (Anesthesiology, 2025) report findings from the multicenter J-PEDIA study analyzing 17,007 pediatric airway management encounters, demonstrating an overall adverse event rate of 2.0%, with respiratory events in 1.1% and desaturation in 2.3%. Neonates and infants had the highest risk, particularly in the presence of difficult airway features or recent respiratory infection. Importantly, first-attempt use of supraglottic devices and administration of muscle relaxants were associated with reduced complication rates, supporting structured risk stratification and proactive device selection in pediatric difficult airway management.
- Read more about this study HERE.
Granell Gil et al. (Current Opinion in Anaesthesiology, 2026) summarize updated EACTAIC thoracic group recommendations emphasizing structured preoperative airway assessment, routine videolaryngoscopy for double-lumen tube placement, and individualized selection between double-lumen tubes and bronchial blockers for lung isolation. The review highlights increasing use of camera-integrated double-lumen tubes, bronchoscopic confirmation of positioning, and specific strategies for predicted difficult airways, including awake fiberoptic-guided bronchial blocker placement.
- Read more about this study HERE.









