Learning objectives
- Describe the importance of postoperative pain management
- Assess postoperative pain
- Manage postoperative pain
Background
- Adequate postoperative pain management is essential to enable a quick return to normal function
- Uncontrolled pain increases sympathetic activity and the stress response, leading to multisystem consequences (e.g., hyperglycemia, immunosuppression, increased risk of myocardial ischemia)
- Pain after abdominal or thoracic surgery can lead to splinting of the diaphragm and chest wall, resulting in decreased lung volumes, atelectasis, poor cough, sputum retention, infection, and hypoxia
- Pain can reduce mobility and increase the risk of thromboembolism
- Psychological effects: anxiety, feeling of helplessness
- Untreated or inadequately treated postoperative pain can lead to chronic pain
- Traditionally, opioids were the standard treatment for postoperative pain
- Today, multimodal approaches for pain management are the treatment of choice
Pain assessment
- Perform pain assessment at regular, frequent intervals and after every intervention
- The severity of pain and the effectiveness of analgesia determine the frequency
- Record pain as the fifth vital sign
- Assessment includes:
- Site, circumstances associated with onset
- Character
- Intensity (at rest and on movement)
- Associated symptoms (e.g., nausea)
- Effect on activity and sleep
- Relevant medical history
- Other factors influencing the patient’s treatment
- Current and previous medications and analgesic strategies
- Severity scales:
- Unidimensional
- Numeric (numeric rating scales, visual analog scale)
- Categorical (verbal descriptor scale)
- Multidimensional (less useful in acute postoperative pain)
- McGill Pain Questionnaire
- Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) can be used to identify those at risk of developing chronic neuropathic pain
- Pictorial and behavioral scales may be needed for children or cognitively impaired patients
- FLACC scale
- Abbey pain scale
- Unidimensional
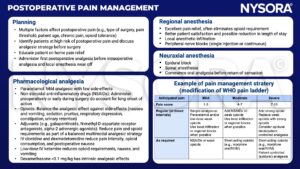
Pain management strategy
Pain in special circumstances
- Opioid-dependent patients (long-term opioids for chronic pain, opioids for cancer pain, recreational use)
- Manage patient expectations
- Provide adequate analgesia
- Prevent or manage withdrawal symptoms
- Acute neuropathic pain after surgery
- Incidence depends on type of surgery (e.g., 85% following limb amputation)
- Pre-emptive analgesia (regional techniques, ketamine, administration before start of surgery) may be helpful
- Maintain a high index of suspicion for patients at high risk
- Treatment is extrapolated from chronic neuropathic pain treatment: Tricyclic antidepressants, ketamine, anticonvulsants, lidocaine, and tramadol may have a role
Suggested reading
- Horn R, Kramer J. Postoperative Pain Control. [Updated 2022 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544298/
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Tharakan L, Faber P. Pain management in day-case surgery. BJA Education. 2015;15(4):180-3.
We would love to hear from you. If you should detect any errors, email us [email protected]








