Learning objectives
- Definition of transurethral resection of the prostate (TURP) syndrome
- Management of TURP
Definition and mechanisms
- Benign prostatic hyperplasia (BPH) occurs in over
- 40% of men aged over 60 years and prostate resection is the second-line treatment if BPH symptoms are resistant to medical management
- Transurethral resection of the prostate (TURP) syndrome is a rare but potentially life-threatening complication of transurethral resection of the prostate procedure
- During the procedure, the prostate at the bladder neck is shaved away
- As the body of the prostate is removed, veins are exposed, but the capsule is maintained
- The exposed veins can bleed, causing significant blood loss, and can also absorb large amounts of irrigation fluid resulting (1.5% glycine solution) in TURP syndrome
- Treatment is largely supportive and relies on the removal of the underlying cause and organ and physiological support
- Mortality is 0.2-0.8%
- Pre-operative prevention strategies are extremely important
Signs and symptoms
- Signs and symptoms are often vague and non-specific as there is no classical TURP presentation
- Symptoms result from fluid overload and disturbed electrolyte balance, and hyponatremia
Central nervous system Restlessness
Headache
Nausea and vomiting
Confusion
Visual disturbances
Cerebral edema
Seizures
Coma
Cardio-respiratory Bradycardia
Hypotension or Hypertension
Tachypnea
Hypoxia
Cyanosis
Pulmonary edema
Systemic Hypothermia
Abdominal pain and distension
Complications of TURP procedure
- Retrograde ejaculation
- Urinary incontinence
- Erectile dysfunction
- Urethral strictures (narrowing of the urethra)
- Bleeding
- Urinary tract infection
- Urinary retention
Risk factors
- The size of the opened venous sinuses
- The amount of irrigation fluid used
- The use of excess amounts of hypotonic intravenous fluids
- Duration of the resection (> 1 hour)
- Perforation of the bladder
Diagnosis
- Acutely unwell, confused patient with a reduced Glasgow Coma Scale score
- Hyponatremia: Na < 120 mmol/L
- Hyperkalemia: K > 6.0 mml/L
- Glycine toxicity
- Intravascular hemolysis
- Disseminated intravascular coagulation
Prevention
- Regional anesthesia is preferred over general anesthesia
- Avoid large amounts of glycine-containing fluid infusion
- Keep the length of surgery under 1 hour
- Keep the patient horizontal and avoid the Trendelenburg position
- Resect large prostates in staged procedures to avoid prolonged operative times
- The optimal height of the irrigation fluid bag above the patient is 60 cm
Management
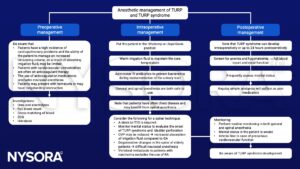
Treatment of TURP syndrome
- Stop the procedure as soon as possible
- Provide oxygenation (intubation) & circulatory support (inotropes)
- Perform invasive monitoring if hemodynamically unstable
- Treat hypotension
- Correct hyponatremia
- Treat fluid overload with diuretics
- Manage disseminated intravascular coagulation
- Perform regular blood tests to monitor improvement in the clotting status
- Control seizures with benzodiazepines
- Treat nausea and vomiting with antiemetics
Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Nakahira, J., Sawai, T., Fujiwara, A., Minami, T., 2014. Transurethral resection syndrome in elderly patients: a retrospective observational study. BMC Anesthesiology 14, 30.
- Demirel I, Ozer AB, Bayar MK, Erhan OL. TURP syndrome and severe hyponatremia under general anaesthesia. BMJ Case Rep. 2012;2012:bcr-2012-006899.
- O’Donnell AM, Foo I. 2009. Anaesthesia for transurethral resection of the prostate. Continuing Education in Anaesthesia Critical Care & Pain. 9;3:92-96.
We would love to hear from you. If you should detect any errors, email us <a href=“mailto:customerservice@nysora.com”>customerservice@nysora.com</a>







