Learning objectives
- Knowing the challenges in the perioperative management of patients with multiple sclerosis
Definition and mechanisms
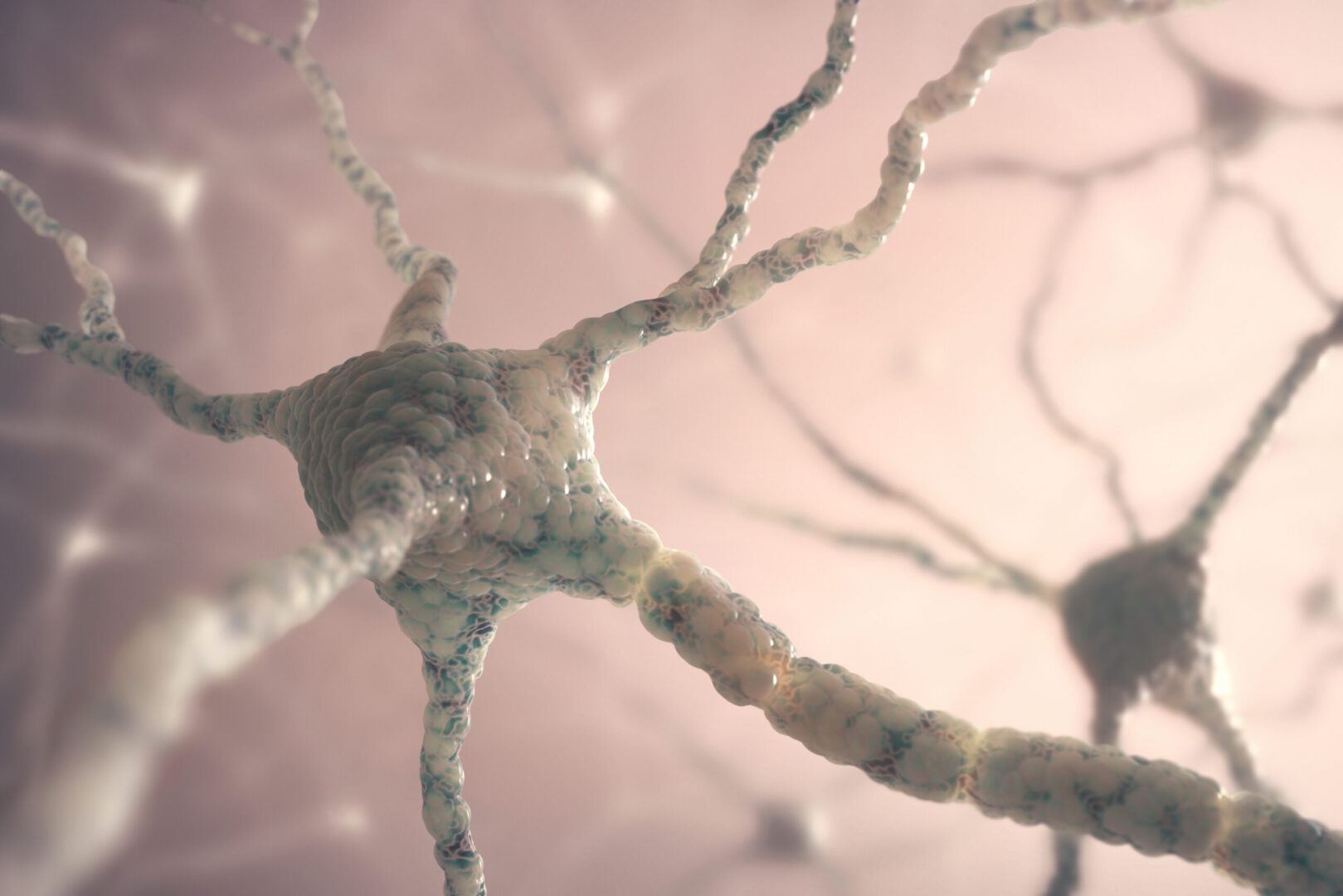
- Multiple sclerosis is a chronic disabling demyelinating inflammatory disease of the central nervous system
- It involves demyelination in scattered areas of the central nervous system
- This leads to the slowing of conduction along the affected neural pathway
- More often in women, it usually presents its first symptoms between the ages of 20 and 40
- Cause is unknown, the most widely accepted theory is of an inflammatory immune-mediated disorder
- There are different types:
- Primary-progressive MS
- Secondary-progressive MS
- Relapsing-remitting MS
- Diagnosis is based on McDonald’s criteria
- Management is multidirectional
- Therapy of exacerbations:
- Corticosteroids
- Prevention of exacerbations:
- Immunomodulatory therapy: interferon beta, glatiramer, Alemtuzumab
- Therapy of chronic symptoms:
- E.g., spasticity: baclofen
- E.g., pain: anticonvulsants
- E.g., urinary incontinence: oxybutynin
- Therapy of exacerbations:
Physiological changes
Symptoms vary depending on the nerve fibers affected:
| Respiratory | FRC ↓, diaphragmatic paralysis, central control of ventilation is altered, risk of chronic aspiration (due to cranial nerve involvement with impaired control of pharyngeal and laryngeal muscles) Increased incidence of obstructive sleep apnea |
| Autonomic nervous system | Hemodynamic instability Syncope, impotence, bladder and bowel dysfunction, vasomotor instability, orthostasis |
| Neurological | Sensory deficits: numbness, tingling, itching of the extremities or trunk. Impairment of facial sensation, trigeminal neuralgia, hemifacial spasms, facial myokymia Cerebellar involvement: tremor, scanning speech, coordination defects, nystagmus, unsteady gait Motor deficits: paraparesis, paraplegia, spasticity, increased deep tendon reflexes Cognitive impairment Increased incidence of epilepsy Fatigue Depression, bipolar disease Pain |
| Visual | Optic neuritis: (unilateral) scotoma, painful eye movements, double or blurred vision |
| Urological | Bladder dysfunction |
Anesthetic management
- Perioperative stress or anesthesia are often implicated as causes of exacerbation of the disease
- Infection, emotional lability, and hyperpyrexia may explain the increased frequency of multiple sclerosis exacerbation postoperatively

Suggested reading
- Makris A, Piperopoulos A, Karmaniolou I. Multiple sclerosis: basic knowledge and new insights in perioperative management. J Anesth. 2014;28(2):267-278.
- A. R. Doratta and A. Schubert. Multiple sclerosis and anesthetic implications. 2002 Curr Opin Anesthesiol 15:365-370.
Clinical updates
Ioannopoulos et al. (EJA, 2025) report in a systematic review of 8 studies (1315 parturients) that neuraxial anaesthesia or analgesia does not increase postpartum relapse rates in women with multiple sclerosis within 12 months after delivery. Across all included studies, relapse risk was instead significantly associated with disease activity during pregnancy or in the year preceding conception, while anaesthetic technique (epidural, spinal, or combined spinal–epidural) showed no independent effect on relapse incidence. These findings support the safety of neuraxial techniques in MS parturients and suggest that postpartum relapse risk is driven by pre-existing inflammatory activity rather than anesthetic exposure.
- Read more about this study HERE.