Learning objectives
- Define inflammatory bowel disease
- Describe the differences between Crohn’s disease and ulcerative colitis
- Anesthetic management of a patient with inflammatory bowel disease
Definition and mechanisms
- Inflammatory bowel disease (IBD) is a term for two conditions (Crohn’s disease and ulcerative colitis) that are characterized by chronic inflammation of the gastrointestinal (GI) tract
- Prolonged inflammation results in damage to the GI tract
- Caused by an interaction of environmental and genetic factors leading to immune responses and inflammation in the intestine → autoimmune disease
| IBD | Crohn’s disease | Ulcerative colitis |
|---|---|---|
| Affected location | Can affect any part of the GI tract (from mouth to anus), most often affects the portion of the small intestine before the large intestine (i.e., ileocecal region) | Restricted to the large intestine (colon) and rectum |
| Damaged areas | Damaged areas appear in patches that are next to areas of healthy tissue | Damaged areas are continuous (not patchy), usually starting at the rectum and spreading further into the colon |
| Inflammation | Inflammation may reach through the multiple layers of the walls of the GI tract → transmural inflammation leading to abscesses or granulomatous disease | Inflammation is present only in the innermost layer of the lining of the colon (i.e., mucosa) → loss of colonic mucosa |
Signs and symptoms
- Persistent diarrhea
- Fatigue
- Abdominal pain and cramping
- Rectal bleeding, bloody stools
- Reduced appetite
- Unintended weight loss
Complications
Both conditions
- Anemia (due to prolonged GI bleeding, often iron and/or vitamin B12 deficiency)
- Colorectal cancer
- Skin, eye, and joint inflammation (e.g., iritis/uveitis, ankylosing spondylitis)
- Medication side effects (e.g., infections, corticosteroids are associated with a risk of osteoporosis and hypertension)
- Primary sclerosing cholangitis
- Blood clots (i.e., venous thromboembolism [VTE])
- Severe dehydration
Crohn’s disease
- Bowel obstruction
- Malnutrition
- (Perianal) fistulas, may form an abscess
- Anal fissure
Ulcerative colitis
- Toxic megacolon
- Perforated colon
Risk factors
- Age
- Most people are diagnosed before 30 years of age
- Some people do not develop the disease until their 50-60s
- White ethnicity
- Family history
- Smoking
- NSAIDs medications (e.g., ibuprofen, naproxen sodium, diclofenac sodium)
Diagnosis
Combination of endoscopy (for Crohn’s disease) or colonoscopy (for ulcerative colitis) and imaging studies
- Contrast radiography
- MRI
- CT
- Stool samples
- Blood tests
Treatment
- Antidiarrheal medications (i.e., psyllium powder, methylcellulose, loperamide)
- Anti-inflammatory drugs (i.e., glucocorticoids, 5-aminosalicylic acids)
- Immunosuppressants (i.e., cyclosporine, azathioprine, mercaptopurine, methotrexate)
- Antibiotics (i.e., ciprofloxacin, metronidazole)
- Biologics (i.e., TNF-α inhibitor infliximab)
- Nutritional support
- Surgery to remove damaged parts of the GI tract
Management
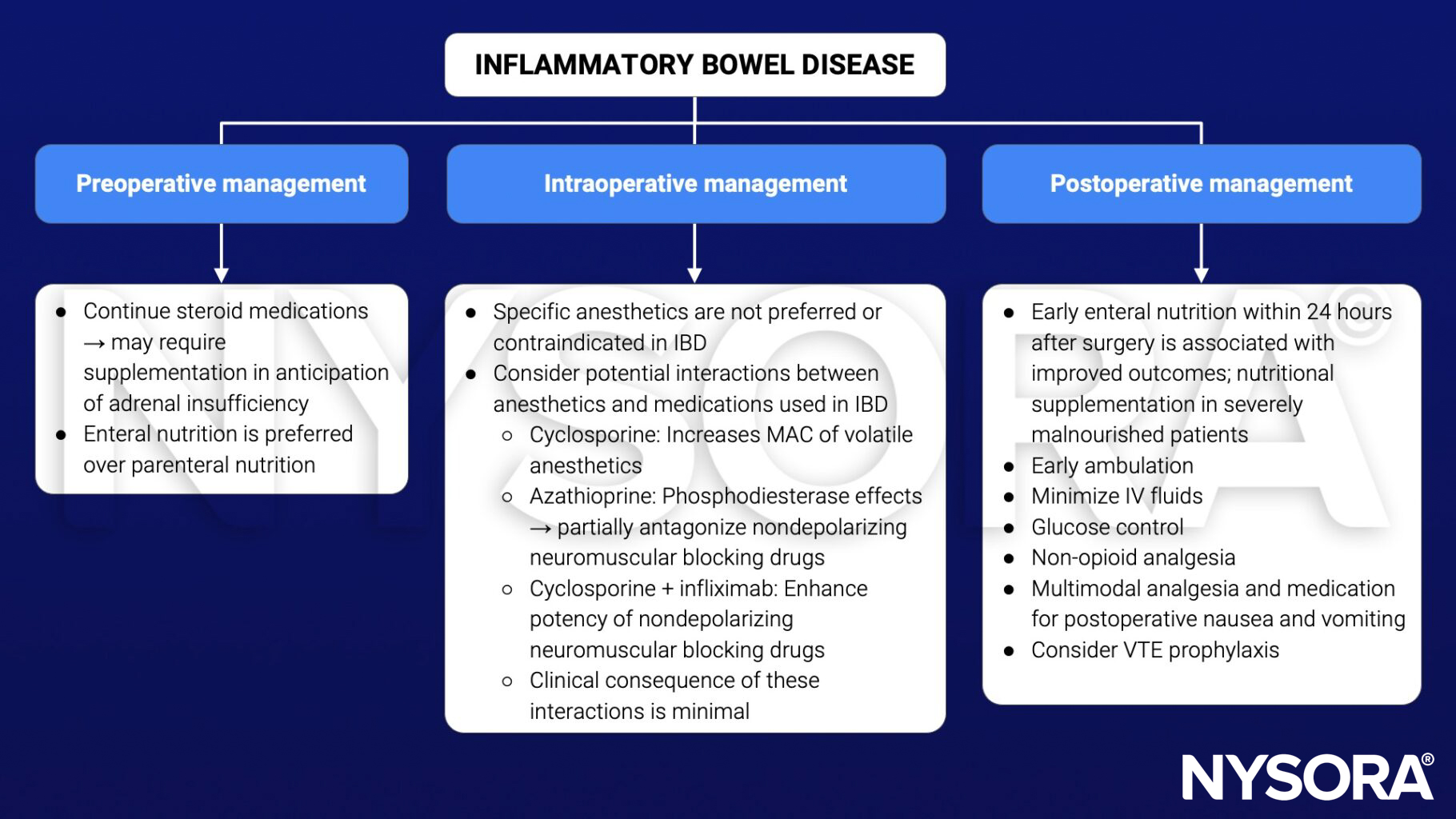
IBD medication management during the perioperative period
| Drug | Recommendation |
|---|---|
| Glucocorticoids | Continue; administer stress dose (see next table) |
| 5-aminosalicylic acid | Discontinue on day of surgery and resume 3 days after surgery if normal renal function |
| Azathioprine, 6-mercaptopurine | Discontinue on day of surgery and resume 3 days after surgery if normal renal function |
| Methotrexate | Continue unless previous poor wound healing or postoperative infections |
| Cyclosporine | Continue but carefully monitor for infectious complications |
| Infliximab | Continue without interruption |
Glucocorticoid management during the perioperative period
| Axis suppression | Minor surgical stress | Moderate surgical stress | Major surgical stress |
|---|---|---|---|
| No Prednisone < 5 mg/d Glucocorticoids < 3 weeks Negative corticotropin test | Daily dose No supplementation | Daily dose No supplementation | Daily dose No supplementation |
| Documented or suspected Prednisone > 10 mg/d for > 3 weeks Positive corticotropin test | Daily dose No supplementation | Hydrocortisone 50 mg IV (induction) 25 mg IV every 8 hours for 24-48 hours | Hydrocortisone 100 mg IV (induction) 50 mg IV every 8 hours for 24 hours 25 mg IV every 8 hours for 24-48 hours |
| Unknown Prednisone 5-10 mg ≥ 3 weeks | Daily dose No supplementation | Positive corticotropin test Hydrocortisone 50 mg IV (induction) 25 mg IV every 8 hours for 24-48 hours | Hydrocortisone 100 mg IV (induction) 50 mg IV every 8 hours for 24 hours 25 mg IV every 8 hours for 24-48 hours |
See also perioperative steroids considerations
Suggested reading
- Nickerson TP, Merchea A. Perioperative Considerations in Crohn Disease and Ulcerative Colitis. Clin Colon Rectal Surg. 2016;29(2):80-84.
- Kumar A, Auron M, Aneja A, Mohr F, Jain A, Shen B. Inflammatory bowel disease: perioperative pharmacological considerations. Mayo Clin Proc. 2011;86(8):748-757.
Clinical updates
Arnal-Velasco et al. (BJA, 2025) publish European multidisciplinary SAFEST consensus recommendations that update perioperative care for high-risk medical patients, such as those with inflammatory bowel disease, emphasising structured preoperative optimisation, medication safety, and complication prevention rather than disease-specific drug changes. Key updates relevant to IBD include stronger endorsement of venous thromboembolism risk assessment and extended prophylaxis, perioperative blood glucose monitoring, early removal of invasive devices, and early postoperative oral intake when gastrointestinal integrity allows, aligning with ERAS principles increasingly applied to IBD surgery.
- Read more about this study HERE.