Learning objectives
- Describe the clinical features of mitochondrial disease
- Diagnose and treat mitochondrial disease
- Manage patients with mitochondrial disease presenting for surgery
Background
- Mitochondrial disease refers to a group of genetic disorders affecting the mitochondria
- Results in complex multisystem disease with varying degrees of severity
- Can present with a wide range of symptoms
- Organs and tissues that have a high ATP turnover are proportionally affected
- Associated with elevated lactate levels
Clinical features
| System | Features |
|---|---|
| Neurological/myopathic | Developmental delay |
| Regression | |
| Weakness | |
| Fatigability | |
| Hypotonia | |
| Spasticity | |
| Ataxia | |
| Seizure disorders | |
| Cardiovascular | Cardiomyopathy |
| Conduction abnormalities | |
| Respiratory | Central hypoventilation/apnea |
| Respiratory muscle weakness | |
| Ophthalmic | Ophthalmoplegia |
| Retinal depigmentation |
|
| Optic atrophy | |
| Renal | Renal insufficiency |
| Hepatic | Hepatic insufficiency |
| Metabolic | Intermittent/persistent lactic acidemia |
| Endocrine | Diabetes mellitus |
| Hypoparathyroidism | |
| Hematological | Macrocytic anemia |
| Neutropenia | |
| Thrombocytopenia |
Diagnosis
Diagnostic test Signs of mitochondrial disease
Genetic testing Genetic defects affecting the mitochondria
Muscle biopsy Ragged-red fibers
cytochrome C-oxidase negative fibers
Biochemical analysis Elevated lactate levels
Brain MRI Strokelike lesions in nonvascular distributions
Diffuse white matter disease
Bilateral
involvement of deep grey matter nuclei in the basal ganglia, mid-brain and/or brainstem
Lactate doublet
Treatment
- Not curative, treatment is largely supportive
- Exercise improves symptoms and increases mitochondrial content and oxygen uptake
- Nutritional supplementation of multiple vitamins and cofactors including:
- Coenzyme Q10
- Alpha-lipoic acid
- L-carnitine
- Creatine
- B-vitamins
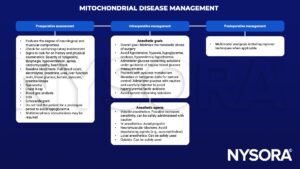
Management
Suggested reading
- Desai, V. (2021). Mitochondrial disease and anaesthesia : WFSA – resources. Mitochondrial Disease and Anaesthesia. Retrieved February 16, 2023, from https://resources.wfsahq.org/atotw/mitochondrial-disease-and-anaesthesia/.
- Hsieh VC, Krane EJ, Morgan PG. Mitochondrial Disease and Anesthesia. Journal of Inborn Errors of Metabolism and Screening. 2017;5:2326409817707770.
- Niezgoda J, Morgan PG. Anesthetic considerations in patients with mitochondrial defects. Paediatr Anaesth. 2013;23(9):785-793.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com